Part 3: Other information
3.1 Indicators selected by the Board in consultation with stakeholders
The Quality Account Regulations specify that part three of the quality account should be used to present other information relevant to the quality of the relevant health services provided or sub-contracted by the Trust during 2022/2023.
Unless otherwise stated, all data for local quality indicators is gathered and reported internally.
As per the requirements for an NHS Foundation Trust, the following is presented:
- An overview of the quality of care offered by the Trust, based on performance in 2022/2023 against indicators selected by the Board, in consultation with stakeholders, with an explanation of the underlying reason(s) for selection. The indicator set selected includes:
- Early intervention in psychosis (EIP): people experiencing a first episode of psychosis treated with a NICE-approved care package within two weeks of referral (the proportion of people experiencing first episode psychosis or ‘at risk mental state’ who wait two weeks or less to start NICE recommended package of care).
- Inappropriate out-of-area placements for adult mental health services (the total number of bed days patients have spent inappropriately out of area).
- Historical data and benchmarked data, where available, so the reader can understand progress over time and performance compared to other providers.
- Reference to the data sources for the indicators, including whether the data is governed by standard national definitions.
- Confirmation is made that all indicators for 2022/2023 are the same as those reported in the Trust’s 2021/22 quality report; and confirmation is made that the data reported has been checked to ensure consistency with the 2021/22 report.
- For each core indicator the number, percentage, value, score or rate (as applicable) for the last two reporting periods is the minimum required; and the Trust has presented data, where available, for the last eight reporting periods.
- Limited data has currently been made available by the NHS Digital but, where this is available, a comparison for previous reporting periods has been made of the numbers, percentages, values, scores or rates of each of the Trust’s indicators with:
- The national average for the same; and
- Those NHS trusts and NHS foundation trusts with the highest and lowest for the same.
The table below details the selected indicators and includes performance against the two mandated indicators (EIP access to care and Inappropriate out of area admissions). The local mandated indicator performance is shown afterwards.
The source for the following data is from Trust systems unless otherwise stated.
Any indicator previously reported in Part 2 have not been repeated here.
| Patient safety | 14/15 | 15/16 | 16/17 | 17/18 | 18/19 | 19/20 | 20/21 | 21/22 | 22/23 |
| Number of inpatient ligation incidents (**from an anchor point) | 164 (4**) | 204 (6**) | 245 (8**) | 217 (6**) | 504¹ (5**) | 283 (11**) | 252 (5**) | 621 (4**) | 415 (15**) |
| Patient safety | 15/16 | 16/17 | 17/18 | 18/19 | 19/20 | 20/21 | 21/22 | 22/23 |
| Infection control no. of MRSA bacteraemia and C Diff infections (threshold: a de minimis applies) |
0 1 C Diff |
0 0 |
0 0 |
0 0 |
0 0 |
0 0 |
0 0 |
0 0 |
| Clinical effectiveness | 15/16 | 16/17 | 17/18 | 18/19 | 19/20 | 20/21 | 21/22 | 22/23 |
| Early intervention in psychosis (EIP): people experiencing a first episode of psychosis treated with a NICE-approved care package within two weeks of referral | 71.4% | 89.6% | 64.8% | 76.9% | 81.6% | 85.1% | 67%* | 60.6% |
*This is an average of figures to date for this year.
| Patient experience | 15/16 | 16/17 | 17/18 | 18/19 | 19/20 | 20/21 | 21/22 | 22/23 |
|
Inappropriate out-of-area placements for adult mental health services (Average number of bed days per month) |
Not available | Not available |
736.62 (Quarter 4 as a whole period data only) |
578.8 |
820 |
460 |
41 |
102
|
|
Under 16yr olds admitted onto adult wards |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
0 |
|
Delayed transfers of care to be kept at a minimal level (threshold 7.5% or below) |
Target: 7.5% |
Target: 7.5% |
Target: 7.5% |
Target: 3.5% Actual 0.9% |
Target: 3.5% Actual 0.5% |
Target: 3.5% Actual 0.2% |
Target: 3.5% Actual 0.1% |
Target: 3.5% Actual 0.5% |
The Trust considers that their data is as described, as reports are validated against the source system and where evidence from the NHS Digital available, reports are validated against this.
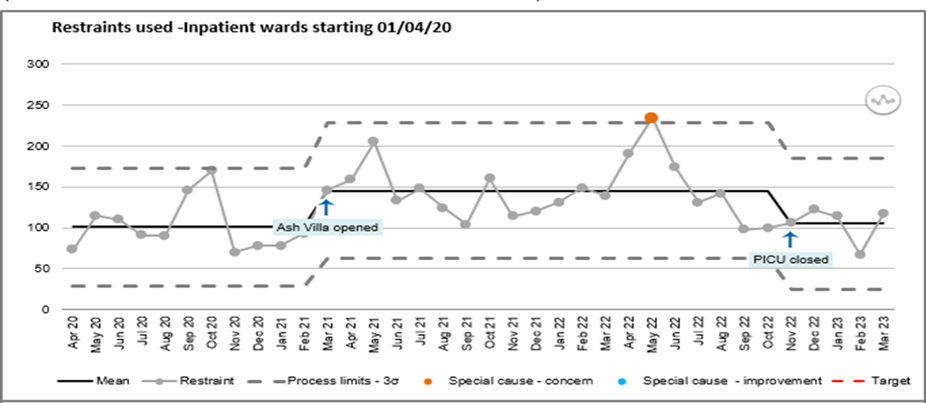
3.2 Local indicator 2022/2023
Reduction in restraint continues to be identified as one of the Trusts local indicators for 2022/2023 with an aim of reducing restraint across inpatient wards by 10%. The Trust strives to build upon its improvement work through a variety of workstreams, however continued changes to the Trust’s inpatient areas, and national pressures, skew the accuracy of the data. It is to be noted that Ash Villa opened in March 2021 and Hartsholme Court (Psychiatric Intensive Care Unit PICU) temporarily closed in November 2022. The data evidenced in the following segment of this report is attributable to inpatient wards only.
For this report the incident reporting categories of violence, abuse and harassment, self-injurious behaviour and self-neglect have been scrutinised.
3.2.1 Restraint
Restraint is defined as the use of physical contact which is intended to prevent, restrict, or subdue movement of any part of the patient’s body. This would include holding a patient to give them a depot injection.
In 2020/2021 there were 943 incidents in which restraint was used. 2021/2022 followed with a sharp increase to 1584 incidents where restraint was used, equating to an increase of 68%. In 2022/2023 there were 1601 incidents in which restraint was used (a 1% increase on 2021/2022).
Number of Restraint Incidents
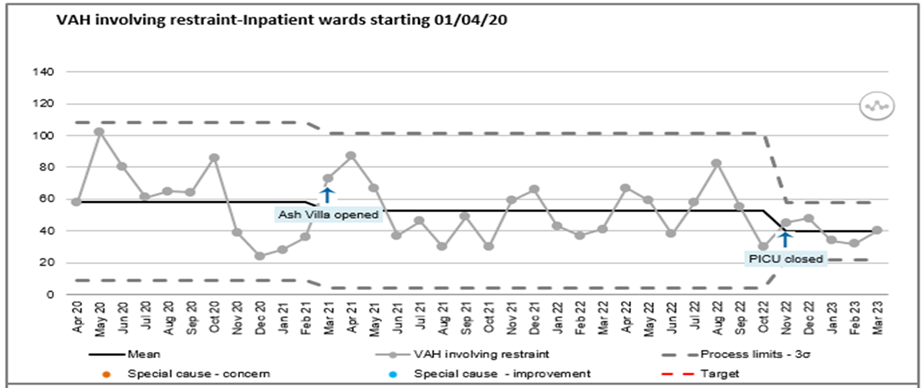
3.2.1.1 Violence, Abuse and Harassment
The total number of incidents of violence, abuse and harassment (VAH) have increased from 2020/2021 reported at 1367 to 2021/2022 at 1544 (13% increase). The total number of VAH incidents occurring on inpatient wards in 2022/2023 was 1858 (a 20% increase).
Restraint, in response to incidents of VAH have decreased, from 716 restraints, equating to 52% of incidents in 2020/2021 to 592 restraints which equated to 38% of incidents in 2021/2022. 2022/2023 saw a continuation of the decrease in restraint used in response to VAH with 593 restraints taking place, which equates to 31%.
Number of Violence, Abuse and Harassment incidents involving restraint
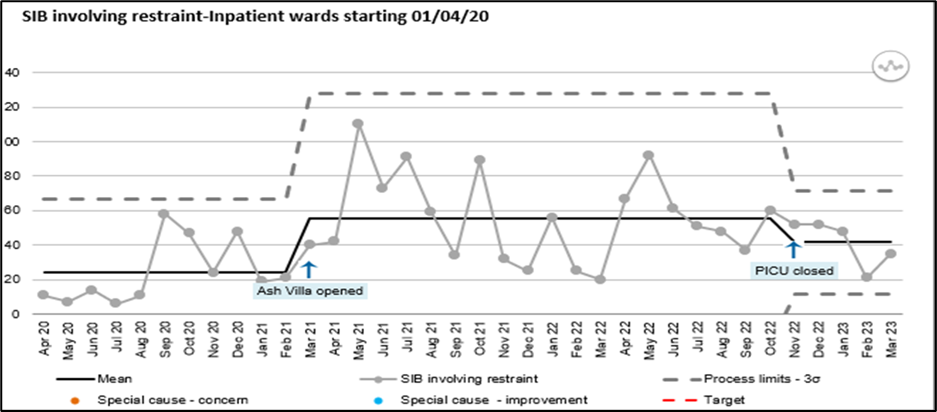
3.2.1.2 Self-Injurious Behaviour
Self-injurious behaviour (SIB) is any behaviour that results in someone causing physical harm to themselves. SIB is often used as a way of dealing with very difficult feelings, painful memories or overwhelming situations and experiences. SIB on the Trust’s inpatient wards can take the form of:
- Headbanging.
- Ligation.
- Occlusion.
- Insertion of foreign objects.
- Swallowing foreign objects.
- Cutting.
- Overdosing.
The above list is not exhaustive.
Occurrences of SIB have seen major rises nationally and this is reflected in the number of incidents experienced in the Trust. In 2020/2021 the number of SIB incidents was 848. This number increased in 2021/2022 by 95% to 1656. 2022/2023 saw a slight decline, by 1%, to 1636 incidents.
To maintain the safety of patients when engaged in SIB, the need for physical restraint is, on occasion, necessary. In 2020/2021 staff were required to intervene on 306 occasions equating to 33% of incidents. In 2021/2022 this rose substantially to 656 occasions, an increase of 114% and equating to 38%. 2022/2023 saw a slight decrease of 4% in the number of SIB incidents requiring physical restraint.
Number of SIB incidents involving restraint
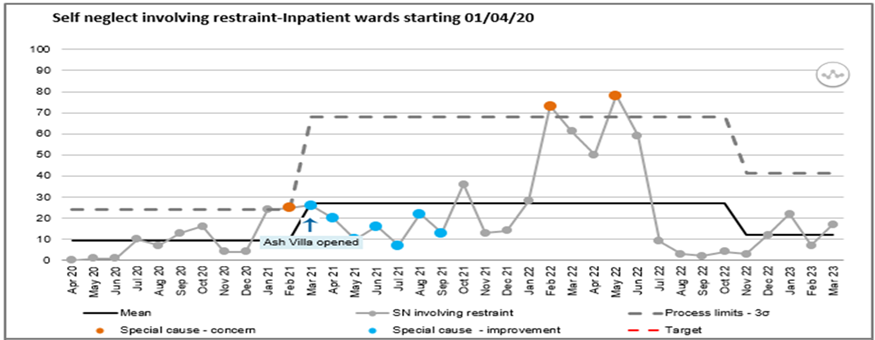
3.2.1.3 Self-Neglect
Self-neglect is a general term used to describe a vulnerable adult living in a way that puts his or her health, safety, or well-being at risk. The two main types of self-neglect that require intervention for patients on the Trust’s inpatient wards are refusal of prescribed medication / treatment and the need to support patients who are refusing to maintain a healthy dietary intake, usually by means of naso-gastric tube feeding.
Interventions to maintain the safety of the patients who self-neglect are carried out on a planned basis to maintain a medication regime or to preserve life via the administration of naso-gastric tube feeding. As a result, this category carries the highest percentage of physical restraint interventions.
The total number of incidents of self-neglect has increased from 181 in 2020/2021 to 352 in 2021/2022, equating to 94%. 2022/2023 saw a 15% decrease in incidents to 266. In order to maintain the safety of the patient, there has been an increasing need to carry out physical restraint, from 56% in 2020/2021, to 86% in 2021/2022 and finally 87% in 2022/2023.
Number of Self-Neglect Incidents involving restraint
3.2.2 Seclusion
Seclusion is defined the supervised confinement and isolation of a patient, away from other patients, in an area from which the patient is prevented from leaving, where it is of immediate necessity for the purpose of the containment of severe behavioural disturbance which is likely to cause harm to others.
In 2020/2021 there were 155 incidents in which seclusion was used following which, in 2021/2022 there were 122 which equates to a 21% reduction. 2022/2023 saw a slight increase of 6% with 128 incidents.
Number of Seclusions
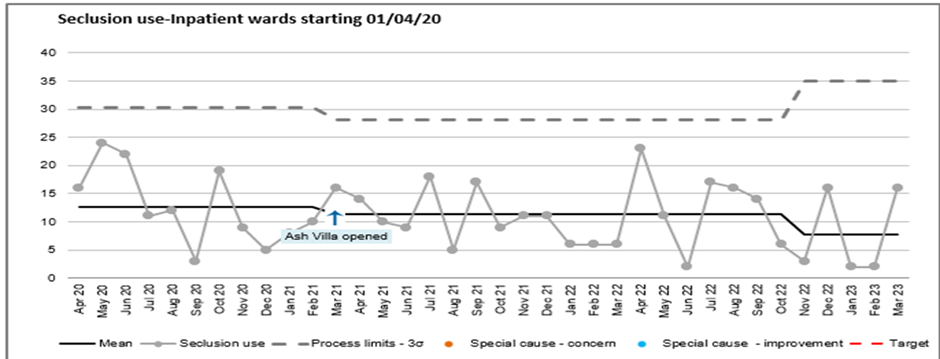
The Seclusion Review Panels continue to be held within 2 weeks of each seclusion and play an integral part in insuring that the use of seclusion is reasonable, proportionate and necessary under the law. The PMVA Team are also in the early days of introducing Restraint Reviews which will be conducted with similar Terms of Reference to the Seclusion Review Panels.
Work aligned to the enactment of the Mental Health Units (Use of Force) Act 2018 is near completion. The Trust’s Prevention and Management of Violence and Aggression Policy, incorporating all policy requirements of the Act, is now available for inclusion in the Clinical Care Policy. Information leaflets pertaining to the Act are now available on the Trust’s SHARON site and care planning requirements, as set out in the Act, have been included in the review of the mandatory Person-Centred Care Plan training.
The Trust has appointed the Director of Nursing, AHPs and Quality as its Responsible Person under the Act. The role is to ensure that the organisation complies with the requirements of the Act.
The Trust continues to contribute to the National Patient Safety Improvement Programme through the Patient Safety Collaborative, within the East Midlands Academic Health Science Network. They are leading the work on the Mental Health Safety Improvement Programme for the East Midlands. This work has been commissioned by NHS England and Improvement (NHSE/I).
The Prevention and Management of Violence and Aggression Team continues to lead local workstreams and projects, through the team’s Restrictive practice Hub and PMVA Working Group, with the focus upon the reduction of restrictive practice within the clinical areas.
3.3 Performance against core indicators
NHSI targets not reported in this table are detailed in section 2.2.9.
The Trust has continued to focus upon delayed transfers of care and implemented a number of strategies into the pathway which have successfully reduced their occurrence.
| 15/16 | 16/17 | 17/18 | 18/19 | 19/20 | 20/21 | 21/22 | 22/23 | |
|
CPA patients having a formal review within 12 months (threshold 95%) |
95.5% |
96.7% |
96.3% |
95.3% |
95.2% |
95% |
95.2% |
70.5% |
|
Improving access to psychological therapies (IAPT) – proportion of people completing treatment who move to recovery (from IAPT) dataset) |
N/A |
53% |
51.3% |
52.5% |
51.3% |
50.7% |
49.7% |
48.3% |
|
Improving access to psychological therapies (IAPT) - Waiting time to begin treatment (from IAPT minimum dataset):
(New description for 2018/19) (New KPI from Quarter 3 2015/16) |
97%
100% |
85.5%
98.8% |
86.5%
98.8% |
88.6%
99% |
88.7%
99.4% |
97.2%
99.9% |
95.6%
99.8% |
96.7%
99.9%
|
| Percentage of people with SMI receiving a full annual physical health check and follow up interventions | This is a new measure provided by NHS Digital for 2022/2023. | 49.4% | ||||||
Whilst the CPA ceased to exist from July 2021 (NHSE, 2021) the Trust have maintained this as a model of care and treatment management whilst formulated a new local framework.
3.4.1 Complaints
3.4 Patient and Carer/Relative experience
3.4.1 Complaints
The Trust is committed to improving the experience that people have when they access our services as either a patient, carer or member of the public. All feedback received, be this positive or not so positive, provides us with the opportunity to review the care and treatment being provided. This allows us to improve the quality of care we deliver, and the experience received.
The Trust has a proactive approach to encouraging feedback. Feedback from comments and complaints enable us to hear the experience that our service users and carers have. Feedback through complaints can be an effective measure of the quality of service delivered and what is needed to improve services and experience. The Trust has a number of feedback mechanisms which we endeavour to meet our service users and carers preferred method of providing feedback. Feedback comes from our everyday interaction with service users and carers by staff working on the front line and our experts by experience and peer support workers who actively seek feedback. A number of our wards have patient and carer groups/sessions to enable staff to respond to concerns immediately and use feedback to change things in their areas.
Feedback highlights any changing trends/demands which is necessary to inform learning. As a learning environment the Trust welcomes this feedback to continually improve the experience and care people receive.
Feedback assists the Trust to:
- Recognise standards of service delivery and continue to ensure service improvement
- Understand the patient experience, perspective and expectations
- Identify any problematic areas
- Identify actions needed
On receipt of a complaint, a risk assessment is undertaken to identify any action that needs to be taken in respect of immediate healthcare/safeguarding needs. This can offer resolution to the concerns raised, for example, contact with the care coordinator, reviewing waiting times, offering an appointment, a second opinion or a change of consultant.
Irrespective of whether a complaint is upheld or not, the Trust demonstrates its responsiveness to that person’s individual experience and offers an explanation from the Trust’s perspective, an apology for any errors which occur, and for the experiences that people have of services provided by the Trust. The Trust also evidences any changes made as a result of a complaint and tracks the progress of these changes.
| Total complaints received | |||||
| 2022/2023 | Q1 | Q2 | Q3 | Q4 | Total |
|
Complaints Received |
41 |
50 |
55 |
46 |
192 |
|
Upgraded from PALS/feedback |
4 |
4 |
5 |
7 |
20 |
| Total | 45 | 54 | 60 | 53 | 212 |
| Total outcomes (resolved) | |||||
| 2022/2023 | Q1 | Q2 | Q3 | Q4 | Total |
|
Not Upheld |
10 |
17 |
11 |
9 |
47 |
|
Partially Upheld |
26 |
28 |
34 |
17 |
105 |
|
Upheld |
5 |
5 |
10 |
7 |
27 |
|
Resolved as PALs |
2 |
1 |
0 |
0 |
3 |
|
Withdrawn |
2 |
3 |
2 |
0 |
7 |
|
Ongoing |
0 |
0 |
3 |
20 |
23 |
| Total | 45 | 54 | 60 | 53 | 212 |
| Total compliance with complaint plan | |||||
| 2022/2023 | Q1 | Q2 | Q3 | Q4 | Total |
|
Met |
36 |
40 |
50 |
29 |
155 |
|
Unmet |
7 |
11 |
5 |
4 |
27 |
|
In Process |
0 |
0 |
3 |
20 |
23 |
| Total | 43 | 51 | 58 | 53 | 205 |
| Primary subject of complaint | |||||
| 2021/2022 | Q1 | Q2 | Q3 | Q4 | Total |
|
Access to Services |
8 |
8 |
10 |
10 |
36 |
|
Appointments |
5 |
2 |
4 |
4 |
15 |
|
Values and Behaviours of Staff |
10 |
10 |
12 |
10 |
42 |
|
Clinical Treatment |
4 |
11 |
9 |
7 |
31 |
|
Communication |
6 |
10 |
10 |
12 |
38 |
|
Prescribing |
2 |
3 |
2 |
1 |
8 |
|
Patient Care |
3 |
4 |
7 |
1 |
15 |
|
Admissions and Discharge |
2 |
2 |
4 |
6 |
14 |
|
Waiting times |
|
|
|
2 |
2 |
|
Trust Administration |
3 |
1 |
|
|
4 |
| Grand total | 43 | 51 | 58 | 53 | 205 |
|
Examples of lessons learned from complaints: |
|
|
You said |
We did |
|
Parent of a child was unhappy that staff were unable to explain the rationale for asking for these details and that it was not clear on the online referral form that they could opt out of providing detailed demographic information |
The team apologised that the administrators did not understand the rationale for asking for demographic information. Additional customer service training has been recommended for staff. The online referral form has been amended so that individuals can indicate if they are choosing not to provide detailed demographic information. |
|
A number of complaints featured issues around not being able to get through on telephone lines at one of our CMHTs. This left people frustrated and angry that they couldn’t reach who they wanted to for a number of reasons including care and treatment, rescheduling or cancelling their appointments |
The team looked into the issued raised and realised that the telephone system had not been able to forward calls internally from external numbers. New software is now in place that allows staff to answer calls through software uploaded on to their laptops. |
3.4.2 Friends and Family Test (FFT)
The Trust continues to actively seek FFT feedback through patient experience feedback questionnaires, including the FFT question, across inpatient and community teams. The real strength of the FFT lies in the follow up questions that are attached to the initial question and the Trust use this rich source of feedback to locally highlight and address concerns.
|
|
2022 |
2023 |
||||||||||
|
Indicator |
Apr |
May |
Jun |
Jul |
Aug |
Sep |
Oct |
Nov |
Dec |
Jan |
Feb |
Mar |
|
How many would recommend % |
87% |
90% |
91% |
91% |
88% |
96% |
89% |
91% |
79% |
93% |
92% |
95% |
3.4.3 Annual Community Mental Health Patient Survey 2022
This is a national survey enabling the Trust to gain a high-level understanding of how patients have responded to a number of questions. The data is used with other feedback, including the analysis of the additional free text comments from the survey, to gain a more comprehensive understanding of themes and patient’s experience overall.
The annual survey compares the Trust with 53 other mental health and learning disability trusts across the country and asks service users their views about the support and care they receive from our Community Mental Health and Crisis Teams. The survey covers 10 sections, including support and wellbeing, organising, planning and reviewing care and medicines.
People aged 18 and over were eligible for the survey if they were receiving specialist care or treatment for a mental health condition and had been seen by the trust between 1 September and 30 November 2021 with the survey fieldwork took place between February and June 2022.
- 1250 people were invited to take part.
- 268 people completed the survey.
- 22% was the Trust response rate which is 1% better than the national response rate.
Survey Findings
The CQC now bands the responses to the questions as much better, better, somewhat better, about the same, somewhat worse, worse or much worse to provide more granular feedback about how the Trust performed compared to other Trusts across England.
Comparison with other Trusts
• About the same as other Trusts in 30 questions
Comparison with 2021 Trust results
• No difference on 20 questions
• Significantly better on 1 question
Where service user experience is best:
- Support and well-being (Work): service users being given help or advice with finding support for finding or keeping work
- Medicines review: NHS mental health services checking how service users are getting on with their medicines *
- NHS Talking Therapies: service users being involved in deciding what NHS talking therapies to use
- Getting help needed: staff delivered help needed at last contact
- Organisation of care: service users feeling their care is organised well
Where service user experience could improve:
- Support and well-being (Physical): service users being given support with their physical health needs
- Crisis care (care): service users getting the help needed when they last contacted the crisis team
- Care review: service users had care review meeting in last 12 months
- Support and well-being (Financial): service users being given help or advice with finding support for financial advice
- Access: service users being seen by NHS mental health services often enough for their needs
|
Patient survey |
Patient response |
Compared with other trusts |
|
Health and social care workers |
6.7/10 |
About the same |
|
Organising care |
8.2/10 |
About the same |
|
Planning care |
6.6/10 |
About the same |
|
Reviewing care |
6.6/10 |
About the same |
|
Crisis care |
6.2/10 |
About the same |
|
Medicines |
7.1/10 |
About the same |
|
NHS Therapies |
7.8/10 |
About the same |
|
Support and wellbeing |
4.5/10 |
About the same |
|
Feedback |
1.9/10 |
About the same |
|
Overview of care and services |
6.6/10 |
About the same |
|
Overall experience |
6.7/10 |
About the same |
|
Responsive Care |
7.6/10 |
About the same |
The Survey also has three sections where patients could make comments in their own words about the care they had personally received. The comments were under the headings of:
- Is there anything particularly good about your care?
- Is there anything that could be improved?
- Any other comments?
The data will be used with other feedback, including the analysis of the additional free text comments from the survey to gain a more comprehensive understanding of themes and patient’s experience overall. This will then be used to triangulate with other data and information to inform our QI approaches.
Responding to the findings
This is a national survey enabling the Trust to gain a high-level understanding of how patients have responded to a number of questions. The data is used with other feedback, including the analysis of the additional free text comments from the survey to gain a more comprehensive understanding of themes and patient’s experience overall.
This year, the Trust looked at a longer-term view across a number of questions from the survey where we had steadily declined in score over the past five years. This will support the Trust to understand where it should focus attention, whilst continuing to improve on areas where we aspire to be better than average.
In the last 12 months, has an NHS mental health worker checked with you about how you are getting on with your medicines? (That is, have your medicines been reviewed?).
The Trust had declined by over 20 points in the preceding two years for service users reporting that they had not had their medicines reviewed in the last 12 months. Actions had been implemented by the Adult Community Division to address this decline which included ensuring materials were produced that encouraged people to raise this with their health professional. Additionally, a QR code was placed on leaflets and posters which guided people to our Medicines Management webpage where they could find out more about medications and where to access further help and information. This is now one of our top five scores.
3.4.4 What service users/patients, carers and the public say
The process for hearing people’s views
There are several formal and informal ways service users/patients, carers and the public can give their views, get involved; and provide feedback. These include:
1. Service user/patient feedback questionnaires (including FFT responses and free text answers)
2. Group of 1,000
3. Complaints, concerns, comments, and compliments
4. Care Opinion website
5. Ward meetings with patients/carers
6. National community survey
7. Expressions of satisfaction
8. Views of the membership and Council of Governors
9. Suggestion boxes
10. Patient reported outcome measures
11. Internal audits
12. Associated Hospital Managers’ hearings
13. Board Stories
14. Voiceability Advocacy drops in and feedback
15. Patient Advisory Liaison Service (PALS)
16. MP enquires
17. 15 Steps Visits
18. Healthwatch Lincolnshire feedback
19. Investigations, including SI investigations
20. Capturing of feedback from service user/patient involvement events/mental health listening events
21. Engagement & Involvement events
22. Formal Consultations
23. Non-executive director and Board member visits
24. CQC inspection visits to clinical areas
25. Peer Support Workers
26. Expert by Experience employed
Please note that some aspects of service user/patient feedback have been reported earlier within this report, including the Community Mental Health Patient Survey results (2022).
Care Opinion
The Trust continues to receive occasional online feedback directly on Care Opinion, and via NHS Choices. Care Opinion is a national independent feedback platform for health services which allows for a conversation between service users/patients, carers, and health service bodies, by allowing people to:
- See what others are saying about the healthcare that each Trust is providing
- Share their story so that others can learn from their experience
- See how health services have responded to comments from others
Care Opinion provides a mechanism for the Trust and healthcare professionals to listen and respond to the experiences of people using this platform. All published opinions go to the CQC and are republished on NHS Choices. Although Care Opinion is available as a form of feedback within the Trust, the Trust needs to give further consideration as to whether it would be beneficial to review its subscription to support increased feedback through this mechanism.
"Communication having all the contact numbers on hand in a crisis. Knowing someone is listening"
"The real good thing is my occupational therapist is really understanding and tries to help as much as she can"
"Seen quickly and put at ease from outset. Was able to talk through issues"
"Impeccable communications, completely non-judgemental, empathetic whilst thoroughly explanatory. Thank you"
"Everyone was supportive and treated me well"
"Professional and sympathetic care especially by veterans services but all staff have been outstanding"
2022-23 Feedback roundup 2022-2023
Friends and Family Test
A nationally mandated test for everyone receiving NHS care
- 91% would rate their experience a good or very good
- Based upon over 5,700 completed FFT surveys which included over 3,100 free text comments
Compliments
Almost 5000 compliments were received during 2022-23 from patients, carers, family members and professionals.
Patient Advice and Liaison
Queries/concerns that can be easily resolved (within 3 working days)
- 152 received in 2022-2023
- 20 of these escalated to complaints
Carers feedback
83 surveys received from carers
- 88% of carers who completed a carers survey reported their experience as a carer as very good or good
- 100% of carers who completed a survey about our carers support services reported their experience as very good
Involvement events
40 involvement events and 11 regular facilitated Focus/Involvement Groups that included 848 participants. Experts by Experience supported 52 interview panels as part of staff recruitment.
Complaints
192 received in 2022-2023 and the top three themes were:
- Values and behaviours of staff
- Communication
- Access to services
These are the same three themes as in 2020-2021 and 2021-2022.
Surveys
Over 1300 other local surveys completed.
Annual Community Mental Health Survey (sent to a random sample of 1250 patients - 22% responded)
Other sources of independent feedback
Including over 50 separate comments received from Care Opinion, NHS Choices and HealthWatch.
3.4.6 Carer/relative developments
Much work has been undertaken, is ongoing or is planned and is summarised in the workplan below for Carer and Relative Experience.
|
Priority area |
Ongoing work |
Already in place/evidence |
Future projects/work |
|
Carers awareness training – Electronic Staff Record (ESR)/F2F Meriden training Confidentiality roadshows Bereavement information updated Carer Lead Induction pack Carer lead monthly forums Orange lanyard identification Triangle of Care accreditation Carers newsletter for staff About My Relative document Carer feedback Teaching students/preceptorship nurses and slot on monthly induction |
Carer boards Orange lanyard posters Carer lead poster List of staff completing training Newsletter 15th edition just completed and available Feedback posters |
Roll out of Confidentiality Roadshows Ongoing Meriden training Reaccreditation for Triangle of Care (ToC) due May 2023 Roll out of About My Relative Document Ongoing Teaching and Induction slots RIO to record carer information and referral to support services through Lincolnshire County Council (LCC) Carer Lead Teams Channel Analysis of ToC Self-Assessment forms to action plan |
|
Carers Council Carers Education and Support Group Interviewing staff Mental Health First Aid (MHFA) training Carers survey to feedback Carers newsletter Triangle of Care info pack Leaflets on website What’s app group Easy referral to Carer Support LCC Carers Charter Carers Strategy Carer Peer support worker Job Description Carers 6-week education courses Carers passport and lanyards Recovery College Courses Long term tech loan Volunteer telephone feedback |
Orange Lanyard poster Orange lanyards to accompany carer passport Carer survey Carer Lead poster
Leaflets Triangle of Care Mental Health crisis Mental Health Act Section 17 Carer Passport Confidentiality Advance Statement Alcohol and Drugs Acronym Buster
|
New Recovery College courses for Carers Long term iPad loan through Tech to Loan Volunteer telephone feedback
New Carer Befrienders through Volunteer service
Upcoming leaflets through Carers Council About My Relative Common Reactions to Grief Ambiguous Grief Deliberate Self Harm Safety and Relapse Planning Trauma Informed Care Abnormal Grief reactions |
|
Staff Carer Forums monthly Staff Carer Register Employment for carers sign up Update on Special leave policy Staff Carer Passport Wider system working |
Staff Carer Forum Poster Staff Carer Register Question in management supervision template Staff Carer Passport Special Leave Policy |
Sign off Staff Carer Passport Add into Electronic Staff Record (ESR) Staff Carer Identification Changes to Special Leave policy to have more info on carers leave Reaccreditation with Carer Confident Benchmarking Scheme (Carers UK) |
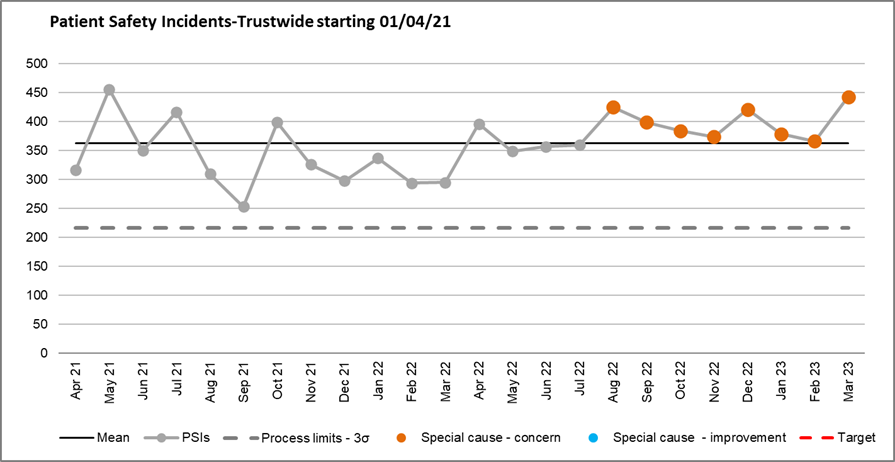
3.5.1 Patient Safety Incidents
3.5 Patient safety
3.5.1 Patient Safety Incidents
Robust systems are in place to manage and support learning from Patient Safety Incidents (PSI’s). Whilst not an indicator of safety in its entirety, incident reporting does provide an opportunity to detect indicators of changes within operational services and across the wider Trust. The Patient Safety Team reviews and monitors all the incidents and data trends reported onto the local risk management system (LRMS) and flags any anomalies. The Team also works closely with the Prevention and Management of Violence & Aggression (PMV) Lead, Matrons, Service managers, Ward managers and Quality Improvement and Assurance Leads to highlight themes and trends and to ensure any required actions are completed. The Patient Safety Team has further developed additional monthly divisional reports to support this increased understanding and thematic analysis of data trends and targeted areas for improvement.
The Trust reports all patient safety incidents to the National Reporting and Learning System (NRLS) to assist with learning both locally and nationally. Whilst it is common practice for most NHS trusts to report to NRLS it is recognised that there are different approaches to reporting and validation of the categories of Patient Safety incidents. The Trust monitors and currently validates all reported patient safety incidents via the Patient Safety Team prior to uploading to NRLS.
For the year 2022/2023 there were a total of 8941 incidents reported by the Trust, of which 4240 were reported to the NRLS as patient safety incidents. Of these 43 were reported as having an outcome of death. After an initial review, 24 of these incidents were considered by the Trust as being possible suspected suicide, of which 3 have returned with a suicide conclusion from the Coroner’s inquest. Cause of death (such as suicide) is confirmed by Coroner conclusions, not the Trust. This can take several months due to the required investigative and coronial processes and this delay, whilst entirely understandable, can be particularly difficult for families affected. In terms of investigating suspected suicides the Trust does not wait for confirmation by the Coroner as prompt investigation and response is desirable.
Patient Safety Incidents-Trust wide starting 01/04/21
3.5.2 Learning from Patient Safety Events (LFPSE)
The transition from the National Reporting and Learning System (NRLS) to the Learning from Patient Safety Events (LFPSE) has been nationally extended to September 2023. In February, the Trust’s local risk management system (LRMS); Datix Web Test was upgraded to be LFPSE compliant, and work is ongoing to review the changes and the impact that will affect all staff in reporting. This also is linked to a sub-group for the Patient Safety Incident Response Framework (PSIRF) around communication and engaging with all trust staff. LFPSE roadshows are planned to engage and consult with frontline staff. The live version of Datix is being upgraded to become LFPSE compliant. AGEM (Arden & Greater East Midlands) and Clinical Systems are actively involved, however staff will not see this in Datix Web Live until the roadshow and engagement has been completed. The Trust is on track to be LFPSE compliant by September 2023.
An Acting Datix Manager is currently in the Patient Safety (From December 2022) to assist with this transition, and the other work linked to this project, such as the procurement process of a new LRMS.
When a serious incident (SI), such as an attempted suicide, suicide, serious assault, or injury, occurs within Trust services it is investigated thoroughly in accordance with the NHS Serious Incident Framework (2015) to learn lessons and reduce or eliminate the risk of such an incident happening again. During 2022-2023 the Trusts Learning from Deaths Lead has continued to lead on all Level 2 investigations to ensure robustness, consistency sensitivity, engagement with patients, families and carers and staff.
The Trust continues to work hard to ensure that patients/service, families, and carers, where appropriate are active participants within SI investigation processes and continually explores ways to strengthen involvement. The Trust has also continued to provide a support for families/carers and staff through a bereavement group facilitated by the Patient Safety Lead and Clinical Investigators. In addition, the Trust has continued to strengthen its support for staff involved in Patient Safety Incidents to ensure that appropriate support in place and that staff feel psychologically and physically safe.
3.5.3 The Patient Safety Incident Response Framework
The Patient Safety Incident Response Framework (PSIRF) sets out the NHS’s approach to developing and maintaining effective systems and processes for responding to patient safety incidents for the purpose of learning and improving patient safety. PSIRF will replace the current Serious Incident Framework (2015). The framework represents a significant shift in the way the NHS responds to patient safety incidents and is a major step towards establishing a safety management system across the NHS. It is a key part of the NHS patient safety strategy.
Implementation of PSIRF is on track. The Trust has a PSIRF Steering Group that meets monthly that discusses the transition through its six phases. The Steering Group has a wide-reaching stakeholder group, including all the Divisions, the key corporate services and ensuring medical engagement. Reporting to the PSIRF Steering Group are currently 3 sub-groups: Communication, Engagement and Involvement and Patient Safety Incident (PSI) Response Standards. There are plans for a further 2 sub-groups, expected to launch in April 2023. Within these sub-groups are divisional engagement and key stakeholders. There is a working group attached to the PSI Response Standards, focussing on improving the support we offer before, during and after an Inquest.
Updates on PSIRF occur monthly with the Director of Nursing, AHPs and Quality (DoN), soon to be extended to both the DoN and the Medical Director from April 2023. The Executive Team (ET) also get bi-monthly updates, via a verbal update with written summaries of each phase. Next ET presentation is in April 2023.
3.5.4 Patient Safety Partners
The Trust has 3 individuals as the Trust’s inaugural PSP’s. One was appointed in December and a further two in March. The first PSP attended induction in March 2023. The PSP working group has been reinstated to ensure a collaborative approach. The oversight and management of the PSP’s responsibility lies with the nominated Patient Safety Specialist.
3.5.5 Reducing suicide and Self-injury in inpatient mental health services
Preventing suicide is complex and no one organisation can tackle the issues in isolation, with this in mind the Suicide Prevention and Self-Injury Lead (SP&SIL) is involved in several projects and working streams across the trust, region and nationally. Including the National Mental Health Improvement Programme. A survey was undertaken to establish how the members of the Suicide and prevention and Self-injury Community of Practice (CoP) will continue as there is now national driver in this area. As it remains a priority for the region and improvement in this area will have great impact into patients’ lives the members agreed a desire to continue with work streams as they are a valuable opportunity to share and learn. It was agreed to continue meeting monthly for the CoP group, but to identify some key pieces of work to progress on for example assessment of risk.
The SP&SIL has started a quality improvement project with services to look at the safer management of self-injury. The SP&SIL has also started work around education for staff and patients regarding safety planning and group clinical reflective sessions to support staff to manage complex self-injury behaviour (SIB). In addition, some wards have introduced higher staffing levels at peak times of SIB’s e.g., twilight shifts, however the effectiveness of this intervention is yet to be evaluated.
3.6 Duty of candour
Every healthcare professional must be open and honest with service users/patients. Every NHS trust, since November 2014, has a statutory duty of candour.
Candour is defined by Sir Robert Francis as: 'The volunteering of all relevant information to persons who have or may have been harmed by the provision of services, whether or not the information has been requested and whether or not a complaint or a report about that provision has been made’.
The being open principles and ethical duty of openness apply to all incidents and any failure in care or treatment. The duty of candour applies to incidents whereby moderate harm, severe harm or death has occurred.
The Trust wants to make this duty a reality for people who come into contact with our services, to ensure there is clear, strong organisational support for staff to follow their ethical responsibility in being open and honest with service users/patients. While the duty applies to organisations, not individuals, individual NHS staff must implement it to ensure that Duty of Candour is met. To support Trust teams with implementing Duty of Candour, the Patient Safety team have held workshops bi-monthly from January 2022 to March 2023, which are open to all members of staff.
The approach of the Trust to Duty of Candour underpins a commitment to providing high quality care, understanding, and sharing the truths about harm at an organisational, as well as an individual level, and learning from them. It is about our organisational values being rooted in genuine engagement of staff, our clinical leadership building on professional accountability, and on every member of staff’s personal commitment to the safety of service users/patients.
The Duty of Candour requirement is outlined in the Trusts policy and overseen by the Patient Safety Team and incident report structure. In the interests of being open and honest, there is the promotion of a culture of transparency that facilitates informing patients and families following any mistake, error regardless of whether it meets the statutory threshold. Robust systems are in place to monitor the Trusts compliance with the Duty of Candour and the Patient Safety Team review all incidents reported onto the local incident reporting system daily to ensure that the Duty of Candour is applied appropriately. All incidents graded as moderate harm and above are confirmed to ensure correct classification as part of the Trust’s obligation under the Duty of Candour. The Patient Safety Team will prompt teams and support staff if required, to contact patients, families, and carers. Support from the Patient Safety Team also comes in the form of an example Duty of Candour letters, and support with writing letters and quality checking when requested by teams.
Latest actions:
The Learning from Deaths Lead has been working with Making Families Count organisation, together with a number of NHS colleagues across a number of organisations to develop documentation and information to support staff and families following incidents. Guidance for staff is available on the intranet; the Duty of Candour Workshop has been refreshed to include a recorded film from families talking about their experiences with Trusts following incidents. To support staff further in understanding their duty and the importance of being open with patients and families, the Learning from Deaths Lead has created a poster to be displayed in all clinical areas across the Trust. The Learning from Deaths Lead is also in consultation with colleagues from another local provider trust to adopt their short 2-minute Duty of Candour video which will be distributed Trustwide.
3.7 Physical Healthcare Team
The Trust remains firmly committed to breaking down the barriers preventing our patients/service users accessing good physical healthcare and providing a caring and compassionate service to all who use our services. The Trust aims to promote good health with equal emphasis on the mental and physical wellbeing of our patients. This is reflected in the Trust Physical Healthcare Strategy 2020-2025.
The Physical Healthcare team are fully committed to working within best practice and national guidelines to ensure our patients/service users receive the highest quality physical healthcare in partnership with both internal teams and wider system partners.
The Trust continues to support our staff by providing guidance and clinical skills in recognition of the deteriorating patient, intervention, and escalation of concerns in a safe and timely manner, and to provide appropriate physical surveillance and monitoring. This continues through the PHILiP (Physical Healthcare Improvements and Learning in Practice) training course and Life Support Plus course. Staff are also supported to gain/develop skills in extended roles including venepuncture, electrocardiogram (ECG) recording, wound care, Prevention and Management of Pressure Ulcers, and Naso Gastric tube feeding where appropriate.
3.7.1 Recruitment
Increasing the support to the teams with meeting patients’ physical healthcare needs is reflected in the increasing size and skill mix of the team. Over the past 12 months recruitment has been successful for the following:
- 0.6 wte Band 7 Highly Specialised Speech and Language Therapist
- 1 x wte Band 6 Tobacco Dependency Treatment Service Clinical Lead
- 1 x wte Band 3 Tobacco Dependency Advisor
- The recruitment process is underway to appoint a Band 4 Nursing Associate to support and facilitate physical health checks for service users with severe mental illness in our community teams.
3.7.2 Physical healthcare Training
The Physical Healthcare Team continue to support and educate staff and patients in many aspects of physical healthcare. They encourage good health practices and support health promotion. They provide clinical nursing expertise for inpatients and outreach advice/support for our Community Teams. We aspire to provide a comprehensive physical healthcare service for all the Trust service users.
Suspension of Physical Healthcare training as a direct result of the Covid-19 global pandemic during 2020 – 2021 was identified as a risk for service users and staff and was added to the Trust risk register – risk no. 154. Training compliance figures have remained lower than the Trust target of 85% despite a recovery plan being put in place to mitigate risks, however significant improvements have been made over the last 12 months.
The Physical Healthcare Improvement Learning in Practice (PHILiP) course compliance figures up to end of Q4 are as below:
| Division | Required | Achieved | Compliance % |
|
274 Adult Community Mental Health (3) |
196 |
130 |
66.33% |
|
274 Adult Inpatient & Urgent Care (3) |
395 |
300 |
75.95% |
|
274 Corporate (3) |
20 |
17 |
85.00% |
|
274 Medical (3) |
2 |
1 |
50.00% |
|
274 Older People & Frailty (3) |
168 |
131 |
77.98% |
|
274 Specialist Services (3) |
259 |
195 |
75.29% |
| Grand total | 1040 | 774 | 74.42% |
The Life Support Plus (for inpatient registered staff) compliance figures to end of Q4 are as below:
| Division | Required | Achieved | Compliance % |
|
274 Adult Inpatient & Urgent Care (3) |
104 |
67 |
64.42% |
|
274 Corporate (3) |
6 |
6 |
100.00% |
|
274 Medical (3) |
14 |
7 |
50.00% |
|
274 Older People & Frailty (3) |
21 |
14 |
66.67% |
| Grand total | 145 | 94 | 64.83% |
The risk is monitored monthly with a recovery plan in place in collaboration with the Learning and Development team. Compliance has improved overall on a month-by-month basis throughout 2022/2023 and it is expected that this will continue over the next reporting period.
The risk has been reassessed and updated to reflect a decrease in status from extreme to high risk but continues to remain a risk until greater numbers of staff who have outstanding competency have attended the course(s) and achieved compliance.
3.7.3 Nutrition and Hydration
Issues around nutrition and hydration in the Trust are monitored via the Nutrition and Hydration Steering Group. This group has been reviewed and is now held jointly with the Physical Healthcare Collaborative to provide robust monitoring. These groups are co-chaired by the Head of Physical Healthcare and the Lead Dietician for the Trust, and representation is well supported by the Divisions. Reporting from these groups is escalated through to the Patient Safety and Experience Committee.
Following extensive discussions between senior leads in the organisation, the decision was taken to transfer the line management of Dietetics services (excluding Eating Disorders Dieticians) from the Specialist services division to the corporate services division. The change came into effect from 1st November 2022 and has been viewed positively by the team members.
Dietetics provision remains unchanged, with the Lead Dietician continuing to line manage the team. Line management of the Lead Dietician has been transferred to the Head of Physical Healthcare.
3.7.4 Inpatient Speech and Language Therapy
Following a successful recruitment process, a Band 7 Highly Specialised Speech and Language Therapist (SLT) commenced in post at the end of August 2022, offering SLT support to all the Trust inpatient services. The postholder is contracted to 0.6 wte and working days are Tuesday – Thursday within core hours.
- A referral process has been put in place and communicated to ward teams.
- Patients in the community (excluding Learning Disability patients) requiring SLT will continue to be referred to the Lincolnshire Community Health Services (LCHS) community service.
- The Trust Dysphagia policy is currently under review and will be presented to the Patient Safety and Experience Committee.
3.7.5 Physical Healthcare in the Community
The life expectancy for people with Severe Mental Illness (SMI) is 15–20 years lower than the general population. Compared with the general patient population, patients with SMI are at substantially higher risk of obesity, asthma, diabetes, chronic obstructive pulmonary disease (COPD) and cardiovascular disease.
People with a long-standing mental health problem are twice as likely to smoke, with the highest rates among people with psychosis or bipolar disorder, (NHS England).
National and regional data suggests that people living with SMI are not consistently being offered appropriate or timely physical health assessments despite their higher risk of poor physical health. They are not being supported to use available health information and advice or to take up tests and interventions that reduce the risk of preventable health conditions.
The NHS Long Term Plan outlines that improved models of community mental health care will include access to physical healthcare to help tackle these unacceptable inequalities in health.
The Trust has recognised that further investment and support is required to increase the uptake and provision of annual physical health checks for our service users and has been working with the Lincolnshire ICB on a strategy to facilitate these as a whole system.
In 2022, a pilot was carried out to run specific Trust Physical Healthcare clinics in Community Mental Health Teams (CMHTs) to test and prove concept to increase uptake of checks by our patients. The outcome was positive, with a proactive model being utilised reaching out to patients to book appointments at the CMHT bases. The appointments were facilitated by members of the Physical Healthcare Team.
A task and finish group were established to improve the delivery of physical health checks to eligible patients with SMI in the community. With support from the Adult Community Division, we have successfully recruited into a fixed term Band 6 1.0 wte Physical Healthcare Practitioner post to support the delivery of annual health checks via a clinic model approach until 31st March 2023.
Ongoing work with the Lincolnshire ICB and Adult Community Division are continuing to further develop and embed processes to sustain improvements made to ensure health checks are received by all eligible service users.
3.7.6 Smoke Free
Work has commenced within the Lincolnshire health system to meet the requirements as set out by the NHS Long Term Plan (LTP) to address tobacco dependency among people with mental health conditions. The NHS LTP commitment for tobacco dependency is to support people to quit smoking. Mental Health inpatients and high - risk outpatients who smoke have been identified as priority groups for this important programme. The LTP aim is that by 2023/2024 all service users in these priority groups will be offered NHS funded tobacco treatment services. It has been recognised that there should be special consideration on rollout to mental health services, where cultural changes relating to treating tobacco dependence may take longer to embed.
Smoking rates among people with a mental health condition are significantly higher than in the general population and there is a strong association between smoking and mental health conditions. This association becomes stronger relative to the severity of the mental health condition, with the highest levels of smoking found in psychiatric in-patients. It is estimated that around 30% of smokers in the UK have a mental health condition, and more than 40% of adults with a serious mental illness smoke.
Work has commenced within the Lincolnshire health system to meet the requirements as set out by the NHS Long Term Plan (LTP) to address tobacco dependency among people with mental health conditions. The NHS LTP commitment for tobacco dependency is to support people to quit smoking. Mental Health inpatients and high - risk outpatients who smoke have been identified as priority groups for this important programme. The LTP aim is that by 2023/2024 all service users in these priority groups will be offered NHS funded tobacco treatment services. It has been recognised that there should be special consideration on rollout to mental health services, where cultural changes relating to treating tobacco dependence may take longer to embed.
Smoking rates among people with a mental health condition are significantly higher than in the general population and there is a strong association between smoking and mental health conditions. This association becomes stronger relative to the severity of the mental health condition, with the highest levels of smoking found in psychiatric in-patients. It is estimated that around 30% of smokers in the UK have a mental health condition, and more than 40% of adults with a serious mental illness smoke.
Data recording metrics have been identified as a requirement for local and national reporting purposes. The Trust Business Intelligence Team are engaged to support and develop mechanisms to capture Patient Level Data for the service. This will be facilitated by the current Electronic Patient Record (RiO). The required data will be submitted monthly from the point of service commencement (2 months in arrears).
To support and consolidate the work of the QUIT team and the service provided, as a Trust we have registered to take part in a national quality improvement initiative hosted by the Royal College of Psychiatrists. The aims of the Quality Improvement in Tobacco Treatment (QuITT) collaborative are to work with every Mental Health Trust in England to support the establishment of tobacco dependency treatment services and increase the number of patients accessing the service. They will also provide opportunities for peer-to-peer learning. This work will also help to inform the roll out of future services.
3.7.7 COVID Booster and Flu Vaccinations for staff
A COVID-19 and Flu vaccination programme was launched with a very clear message of healthcare workers being at increased risk of contracting COVID-19 and flu, as well as being at risk of passing viruses on to the most vulnerable in our community. To make them accessible for staff several ways of getting the vaccines have been available through the Hospital Hubs on United Lincolnshire Hospital sites which offered both the COVID-19 booster and flu vaccine at the same time. Locally hosted clinics by LPFT across bases for the flu jab only, as well as peer vaccinators who are contactable to make alternative arrangements for the flu vaccination and staff obtaining them through GPs. Unfortunately, this has led to significant difficulties in achieving reliable and accurate rates.
The Covid booster and flu vaccination figures for 2022/2023 are detailed below.
|
Type of Vaccination |
Percentage |
|
COVID-19 Frontline uptake |
Unable to access data |
|
COVID-19 Non frontline uptake |
Unable to access data |
|
Flu Frontline uptake |
36.6 % |
3.8 Workforce planning
The Trust engages with the clinical services in developing its approach to workforce through integrated business, finance and workforce planning. The Associate Director of People and Divisional HR Business Partners (HRBPs) attend the business planning meetings alongside service managers and finance colleagues led by the Head of Business Development, in order to explore ways in which vacancies will be addressed. Proposals developed and discussed at business planning meetings will then be presented at People and Workforce Advisory Group (PWAG) to allow for a cross Trust view of annual workforce plans. Proposals are challenged to ensure that they are realistic and deliverable. The Trust recognises that whilst we must maximise attracting people into existing vacancies, grow our own pipelines, we must also consider new pipelines of talent and new roles to ensure safe staffing levels in the future.
The Trust has continued to develop a model to support predictive analytics for vacancies. This report considers predictive turnover, recruitment pipelines and supply pipelines to forecast workforce supply over the following 12 months. This information is then used to inform workforce planning around what is realistically deliverable in terms of staffing increases over the forthcoming year. This vacancy dashboard is used by the HRBP’s to work with their divisions on a plan for every vacancy, to ensure robust recruitment plans are in place. A report including progress against our workforce vacancies and planning is submitted to PWAG, Executive Team and for assurance to the People Committee.
2022/2023 has continued to see a growth in investment in our services. As the graph below shows despite the overall actual Full Time Equivalent (FTE) number of employees having steadily risen, the budgeted FTE has risen more, thus resulting in an increasing variance and therefore an increase in the vacancy rate. This expansion has made the recruitment of registered professionals an increasingly difficult task, especially given the shortages nationally.
Actual and budgeted Full Time Equivalent number of employees
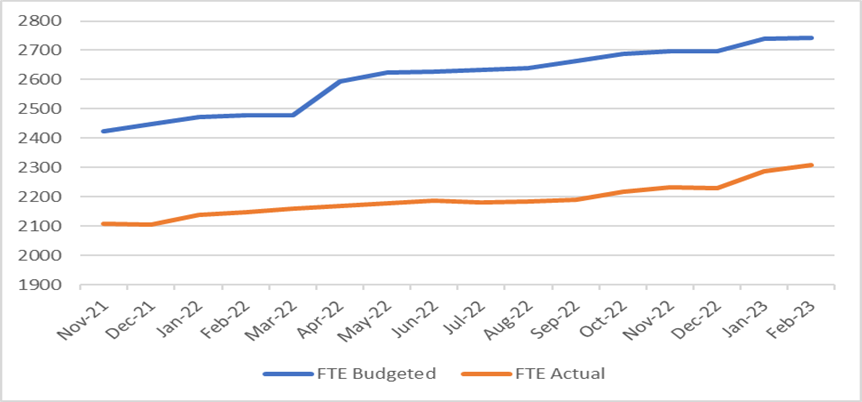
The trust has supported the international recruitment project since summer 2021. We have now welcomed 7 cohorts of international nurses providing us with a total of 23 people of which 17 have passed their OSCE exams and have NMC membership.
The trust has committed to a further programme of international recruitment of nurses, social workers and Health Care Support Workers over the next 3 years with a target of appointing 38 nurses, 13 social workers and10 senior Health Care Support Workers in the next year. 9 nurses are in the pipeline and due to arrive in the summer months and we continue to work with 5 nurses from India identified during the visit to Kerela; one of whom is ready to receive her visa. The remaining are working on their required language and CBT (computer-based test). We have offered 13 Indian social workers posts and we will welcome them through the summer/autumn period into inpatient and community SW and MHP roles.
The international recruitment team won the Trusts Chair Award at the annual excellence awards ceremony in October 2022, recognising the innovative work and contribution to widening diversity of the workforce.
Medical - Workforce Planning
Provision of our established Consultant Psychiatrist medical workforce continues to be challenging and this is mirrored across the NHS, there are currently 295 vacancies on the NHS Jobs website in a range of psychiatry specialities. The Trust has seen staff leave the organisation and remaining medics have taken on additional programmed activities to temporarily fill these gaps. Despite this, we are having some success in recruiting to consultant roles and have 4 Advisory Appointment Committees (AAC) panels taking place in April/May with further adverts to go live shortly.
A review of the establishment has been carried out and we now have a clear picture of the vacancy position agreed with finance colleagues and work is ongoing to align this to ESR.
As part of the recent recruitment event in Kerela in India, we were successful in recruiting five speciality doctors, however, two doctors have since withdrawn their applications. The remaining three doctors are due to join the Trust in May/June 23.
To increase the number of potential future consultants and looking to “grow our own” the Trust is working with The British Association of Physicians of Indian Origin (BAPIO). BAPIO is a voluntary organisation and works with Trusts to recruit international doctors. The Trust is looking to recruit CESR Fellows with BAPIO, supporting them to get specialist registration. This programme will be advertised for both internal and external staff to apply for.
Following on from the success of the initial cohort of Medical Support Workers (MSW) the Trust is hoping to have a second cohort of four MSWs and will work with the refugee doctor programme in Lincolnshire to ensure that these roles are available to refugee doctors. MSWs are doctors who have qualified outside the UK or who haven’t practiced for some time and do not have GMC registration. The aim of the programme is for the Trust to support these MSW to obtain GMC registration.
The Trust is active regionally in preparing for the Physician’s Associates apprenticeship scheme which is due to start in September 2023. A further apprenticeship for Medical Staff is in the pipeline and this will be explored once more details are available.
Along with nursing recruitment, medical recruitment remains a priority within the People and Medical Directorates and active international recruitment will continue into the new financial year as referenced above.
A regular update on staffing and locum usage is provided to Medical Management Team (MMT) for assurance and progress reporting, in addition to the recent establishment of specific monthly workforce medical management meetings, and appropriate monitoring mechanisms. Recruitment versus establishment will always be transient as posts are established and dis-established due to commissioning decisions and the changing landscape in the wider system.
New promotional materials have been developed and in association with system developed materials, the ‘Be Lincolnshire’ branding will help drive interest in the county as a place to live and work.
The junior doctor intake remains active with some vacant posts however, we have filled these with locally employed doctors. The Trust has again received positive feedback as an excellent place to train as a doctor and continues to encourage all trainees to return to the trust on completion of their medical studies.
Growing Own Strategy
Although active recruitment to new roles and new teams is essential, the Trust also encourages career development of its current staff. For a number of years, The Trust has supported non-registered staff to become registered in a number of nursing and non-nursing professions. As of January 2023, the Trust is supporting the following through degree level apprenticeship programmes:
|
|
Completion Year |
|
|||
|
2023 |
2024 |
2025 |
2026 |
Grand Total |
|
|
Advanced clinical practitioner |
5 |
1 |
|
|
6 |
|
Occupational therapist degree |
2 |
2 |
|
2 |
6 |
|
Registered Nurse degree |
12 |
16 |
6 |
9 |
43 |
|
Social Worker degree |
1 |
3 |
2 |
|
6 |
|
Grand Total |
|
|
|
|
61 |
In addition to the degree level apprenticeships shown above we are also supporting 22 Nursing Associate Apprentices who will qualify between July 2023 and September 2025. The clinical divisions continue to value the benefit a nursing associate brings to the team such that most of the clinical areas have the role within their establishment. The nursing associates bring a breadth of physical healthcare to the role, and many choose to further upskill to fully registered mental health nurse on an 18-month apprentice programme.
The Trust’s Bank Staffing Unit (BSU) continues to work closely with the divisions to recruit Registered Nurses (RNs), Allied Health Professionals (AHPs), health care support workers (HCSWs) and administrative staff to the Bank; and to provide a reliable effective service aligned to NHSE/I agency rules. The Trust is currently working with NHS Professionals to implement their National Bank, the aim is to migrate agency staff to the national bank, reducing agency costs as NHSP is more cost effective, staff will also be recorded as bank rather than agency usage.
Safe staffing levels on inpatient wards continues to be a high Trust priority, with safe staffing reviews ensuring good multi-disciplinary ownership, engagement and use of professional judgement. The Trust has continued to invest in a safe care system, which supports the monitoring of safe staffing aligned to patient acuity using the mental health optimal staffing tool Mental Health Optimal Staffing Tool (MHOST) and Care Hours per Patient Day (CHPPD) in line with national guidance. The Trust uses the MHOST which is a licensed, evidence-based tool biannually to review staffing establishments and skill mix.
New Roles
We are embracing new roles and ways of working. We are recruiting for Cohort 3 of the Mental Health Wellbeing Practitioner (MHWP) program which will see 12 students join Derby University for the first time. Once recruited we will have 25 MHWP in Locality teams across the county providing wellbeing interventions.
The training for our internal role of Psychological Intervention Facilitator (PIF) has just concluded for 9 participants and the second cohort is due to start shortly with 10 participants. Feedback from the participants has been very positive a number have expressed an interest in applying for MHWP positions and one has already gained a place on the MHWP training.
We continue to recruit and train Peer Support Workers (PSW) with 7 booked on the most recent round of HEE training, the Trust’s Recovery College is now accredited for the delivery of PSW training.
Demand and Capacity
The mismatch between capacity and demand can lead to increased work pressure and jobs that become untenable. Increasing the Trusts capability to conduct robust capacity and demand analysis has commenced.
The Trust has purchased a number of licences for the Stella Architect software and a cohort of LPFT staff have completed training to use the capacity and demand modelling tool. Work has now commenced to apply the software and learning to a number of service pathways.
Perinatal, Memory Assessment and Management Service (MAMS) and the Healthy Minds service will be the first tranche of pathways to be fully modelled and have detailed capacity and demand analysis conducted. The intention is to have the Perinatal service fully modelled and analysed by June, with MAMS and Healthy Minds being fully completed shortly after. Interdependencies have been identified with other workstreams, in particular the project on Job Planning. For the capacity and demand work to be as accurate as possible, it relies on certain information and the project on job planning will be essential to enable accurate capacity and demand analysis.
Community Job Planning
By documenting activity in job plans the divisions can better understand their workforce capacity for community services and match it to patients’ needs. At present the organisation lacks the ability to articulate the expectations of the workforce, whether ratios around contacts and administration duties are appropriate, and what capacity we have and is required to meet the demand. Introducing job planning will provide clarity around this and enable us design and quantify “doable” jobs, which enables us to understand our capacity and help to limit staff burnout.
In order to enable this programme of work, the Trust have accessed a Workforce Planning Masterclass programme through HEE. This is a blended learning programme which provides a practical guide to sustainable and evidence-based workforce planning. Through the 18-week course which commenced 19 October 2022, we are guided in the use of tried and tested improvement tools and techniques including clinical pathway mapping, skills profiling and competency mapping. Through regular group sessions and facilitated workshops we have access to specialist workforce planners within HEE and opportunities for cross-organisational reflective learning and peer support from two other project teams within our cohort. We have a multi-professional team attending this programme. Learning is being brought back into the wider Trust project group on Community Job Planning and we are sourcing appropriate teams to pilot job planning to start the phased approach to implementation.
3.9 Leadership and Organisational Development
The activity that has taken place is presented below and covers the period April 2022 to March 2023.
|
Programmes delivered/facilitated |
Length of programme |
No. of cohorts |
No. of staff attended |
|
Appraisal Training |
½ day |
6 |
85 |
|
Compassionate Leadership Circles |
1.5 hours |
17 |
83 |
|
Inspirational Leadership Programme (ILP) |
½ day |
4 |
Average of 87 |
|
Leadership Induction |
3 days |
6 |
84 |
|
Leadership Development Programme |
6 days |
5 |
47 |
|
Coaching Skills for Leaders |
1 day |
5 |
33 |
|
Team Time |
½ day |
2 |
N/a |
|
System Coaching Supervisions (Lincolnshire System) |
½ day |
2 |
9 |
|
Stay Conversations |
N/A |
N/A |
8 |
|
Action Learning Sets |
1.5 Hours |
14 |
Average of 9 |
|
B7 Inpatient Development Programme |
7 days |
2 |
15 |
|
Affina Team Journeys |
N/a |
N/a |
15 teams |
|
Affina Coaching Skills |
½ day |
1 |
3 |
|
Coaching |
Number of system coaches |
Number of referrals |
|
|
29 |
47 |
|
SDI – Number carried out in team development, development programmes and 1:1 feedback |
191 |
|
|
360 Appraisal’s carried out |
45 |
Team development/ interventions were delivered to the following teams
- CAMHS Crisis North Team
- Communications
- Executive Team
- Staff Wellbeing Service
- Older Adults & Frailty
- Finance Team
- CAMHS Crisis South Team
- Board Development
- Associate Directors
- Charlesworth Ward
- Young Minds Matter
- Specialist Admin Children and Young People
- Finance Team
- Senior Operations Team
- Speech and Language Therapy Team
- Board Development
- Boston Healthy Minds
- Lincoln Crisis Team
- Research Team
- Bank Staff Unit/Health Roster/Workforce
- NQN's - Preceptorship
- Staff Wellbeing Champions
- Medical Away Day
- CFT
- Horncastle Healthy Minds
- Boston Healthy Minds
- Learning Disabilities Leadership Team
- MHA Team
- Eating Disorders team
- Grantham IPBT
- NQN’s – Preceptorship
- Transforming Care Liaison Team
- Team of Teams - Sleaford IPBT/ NT Link Workers
Over 360 staff have attended, some teams had multiple sessions.
3.10.1 Training
3.10 Learning and Development
3.10.1 Training
In 2022/2023 we have delivered the first full year of training since COVID-19 had an impact on training delivery, which was on and off between March 2020 and January 2022. Although some training has returned face to face some has remained being delivered online through MS TEAMS.
The HCSW development programme has been successfully rolled out, gaining national recognition for it, and staff feedback showing how it increase confidence and knowledge base. There have been some challenges in releasing our HCSW’s to attend a 5-day course however the Practice Educators are working with operational colleagues to look at alternative ways of delivering that will better align with service needs.
Tier 3 suicide awareness has been developed and rolled out face to face for selected clinical staff in patient facing roles. Tier 2 training is for clinical and non-clinical staff in patient facing roles and this continues to go from strength to strength with updates from National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH). Feedback indicates that clinicians find theory of suicidality and case studies particularly useful, giving confidence in assessing suicidality.
Training in the centre
Training in and organised by the centre happens in two ways:
1. Training organised, run and presented by the Sleaford Practice Education Team:
- Induction
- Person-centred care planning
- Suicide and self-harm (Tier 2 and Tier 3)
- PHILiP (Physical Healthcare Improvements and Learning in Practice)
- IROC and recovery training
- Moving and handling
- Mental health first aid (as part of HCSW training)
- Healthcare support worker induction training and care certificate
- Clinical Supervision
2. Courses hosted by the training centre:
- PMVA
- Safeguarding
- Mental Capacity Act
- Information governance
- Mental Health Act training
- Medication management
- Meridian, carers training
International Recruitment OSCE Training
Two Practice Educators (Nurses) continue to support the Trust International Nurse Recruitment Programme to write and present a course to train and coach international nurses to enable them to take and pass the Nursing and Midwifery Council (NMC) Objective Structured Clinical Examination (OSCE). OSCE is a modern type of examination used in assessing nurses for practice and a required standard for international nurses to pass before they can be employed in England. To date 17 international recruits have sat and passed their OSCE exam, which is testament to both the candidates themselves and the Practice Educators.
We have run one 4 days intensive train the trainer programme in December 22 which will enable a number of Trusts to run their own mental health OSCE programme. Cohort 7 consists of two mental health nurses from Sheffield Health and Care Trust working alongside our own recruited nurses.
Courses Delivered
- Clinical Supervision
- Alpha Solway
- BANK Induction
- CAMHS MCA
- Clinical Risk Assessment
- ECG / Venepuncture
- Emergency First Aid at Work
- Fire Marshall Training
- Fire Safety
- Food Hygiene Level 3
- Food Safety Level 2 in Catering
- HCSW Development Programme
- Housekeepers Competency Training
- Immediate Life Support
- Induction
- Infection Control/Hand Hygiene
- Information Governance
- Initial Medicine Management
- Life Support Plus
- Ligature Training
- MCA / Dols Level 3
- Medicine Management Annual Assessment
- Mental Capacity Act Level 4
- Moving & Handling Level 2
- Person Centred Care Planning (PCCP)
- Physical Healthcare Refresher
- Physical Healthcare Training
- PMVA
- Refresher MCA Level 2C (CAMHS ONLY)
- Refresher MCA/DOLS Level 3
- Safeguarding Adults
- Safeguarding Children Level 3B
- Safeguarding Level 2
- Safeguarding refresher
- Safeguarding children
- Suicide and Self Harm Awareness Tier 2
- Suicide Prevention Skills Lab Tier 3
- Triangle of care (carers training)
3.10.2 Continuing professional development (CPD) and Workforce Development Funds (WDF) Money
The Trust’s allocation of CPD funds this year has been £215,333, of which £215.117.90 has been allocated against training. The Associate Director of People and Head of Nursing, Safe Staffing and Professional Development attended DMT meetings at the start of the year to explain the allocation and to ask that divisions consider prioritising spend of this against the priorities that would see maximum impact for the Trust. 96 different types of training opportunity have been procured, for a total of 486 nurses and 255 AHPs. This has been a mixture of training identified by operational divisions as being needed for their nurse and AHP workforce and that identified by individuals as being professional development they wish to pursue, that said it must be supported by their line manager and align to workplace priorities.
2022/2023 is year 3 of a 3-year funding promise for CPD, whilst we do not yet know the monetary value for 2023/2024, we have been informed that there will be a CPD allocation which will be similar to previous years.
LPFT was allocated £26,721 for WDF, which was to be spent on the improvement and transformation of care delivery. As a Trust we have invested £19,500 in training 12 individuals to become accredited Affina Team coaches who will then coach individual teams across the Trust to enable them to work more effectively as true teams. This decision was taken as our Walking in Your Shoes programme showed that the top reason for staying with the Trust was due to effective and supportive teams. In addition, with our transformation programmes we are seeing team composition change and new roles being added to our multi-professional teams. Therefore, investment was channelled into this area to support with retention and the wrap around support required for transformation to be a success. We have also purchased an additional 25 Affina licences to support 25 teams across the organisation. The remaining £4,500 is being used to support with the establishment of a Trust Training Needs Analysis process to enable co-ordinated and targeted training ensuring resources are utilised to have the maximum impact on patient care.
3.10.3 Apprentices
LPFT currently have 119 employees undertaking an apprenticeship, with 61 due to complete in 2023, in comparison with 23 completing in 2022, and 29 completing in 2021. The graph below shows the split of these across disciplines and year of completion, where 2022 is shown as year of completion this is because the apprentice has paused their training. The “other” section includes apprenticeships in customer services, data scientist, healthcare assistant practitioner, electrician, junior energy manager, operation manager, project manager, quality practitioner, senior leader and software development technician.
Current Active Apprentices
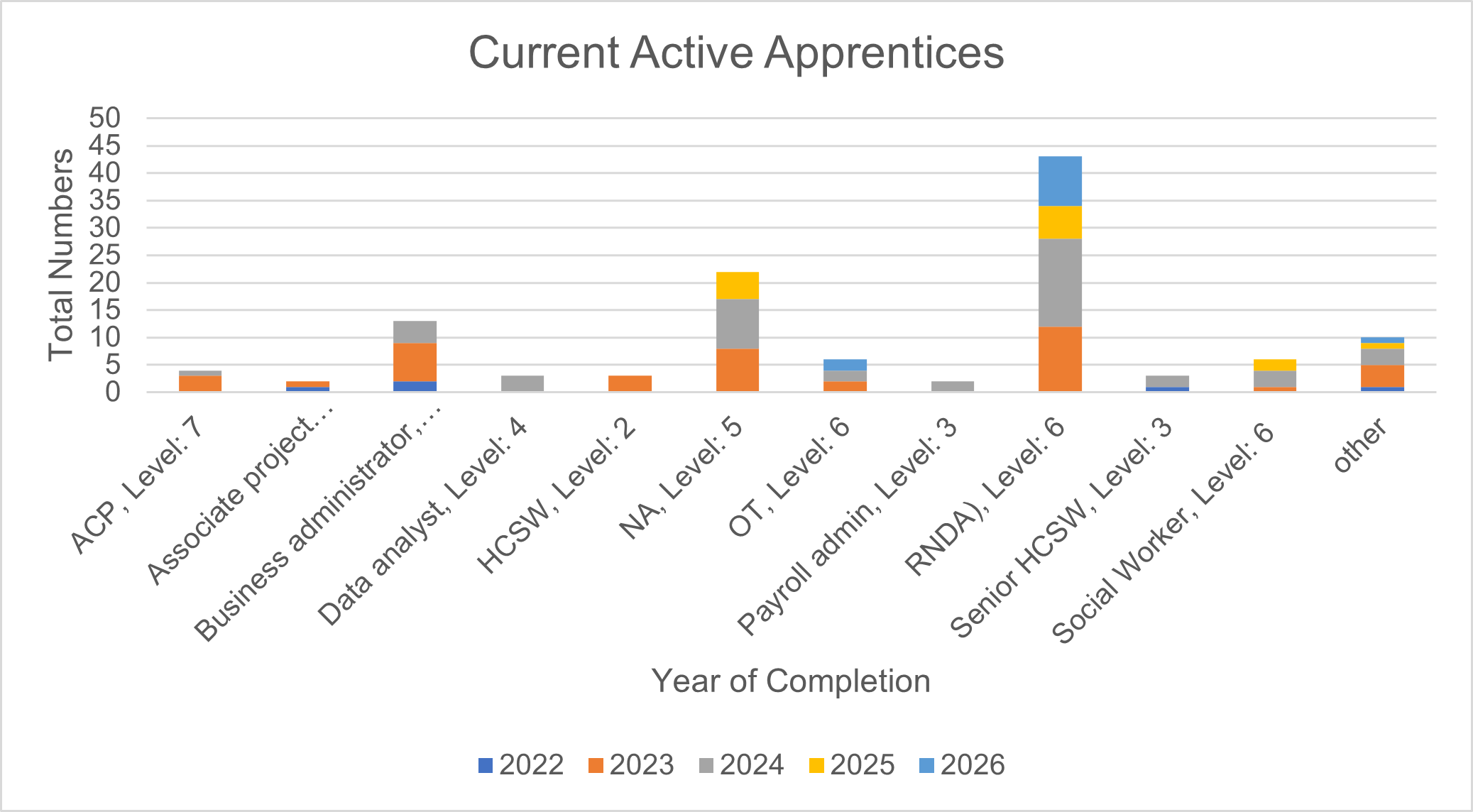
Levy Spend
The Trust’s levy balance, at 21/04/23 is £623,793. In the last 12 months we have spent £563,007 of levy supporting apprentice training and the projection is that we will spend £484,932 in the next 12 months. The projected income for the next 12 months is £625,377.
The Trust has approved appointment of 50 Degree level nurse apprentices per year for the next 3 years to help fill our large nurse vacancy position. This will use all of our levy and we will seek levy transfer from other organisations to support funding this. We are working with HEE in respect of this.
3.10.4 Mandatory Training Compliance
The overall compliance rate for Mandatory training is 90%, which is a strong position to be in. Of all the divisions the Medical Directorate has the lower compliance rate, and this is something our Head of Medical Staffing and our Medical Director are exploring reasons for and planning to address to increase their compliance.
|
|
Community |
Inpatient |
Corporate |
Medical |
OPAF |
Specialist |
|
BLS |
87.75% |
83.87% |
87.19% |
77.27% |
84.26% |
85.68% |
|
Counter Fraud |
96.05% |
92.51% |
94.28% |
80.80% |
93.45% |
95.69% |
|
Prevent |
95.02% |
91.99% |
92.41% |
82.86% |
91.77% |
94.43% |
|
Diversity |
94.90% |
90.59% |
94.28% |
80.80% |
94.18% |
95.32% |
|
Fire |
91.28% |
86.41% |
88.56% |
70.40% |
88.36% |
90.07% |
|
H&S |
94.74% |
90.77% |
95.10% |
79.20% |
95.27% |
96.25% |
|
Infection Control |
94.74% |
95.64% |
93.73% |
80.00% |
93.82% |
94.94% |
|
Information Governance |
92.60% |
87.46% |
92.10% |
76.80% |
90.91% |
93.45% |
|
Moving & Handling |
94.90% |
91.29% |
92.92% |
79.20% |
94.55% |
95.51% |
|
Safeguarding Adults level 1 |
93.91% |
94.77% |
92.92% |
77.60% |
94.55% |
95.51% |
|
Safeguarding Children Level 1 |
95.23% |
95.12% |
93.73% |
80.80% |
94.55% |
96.63% |
|
Overall compliance |
93.80% |
91.10% |
92.59% |
78.61% |
92.51% |
94.15% |
We are at the early stages of procuring a new learning management system to enable easier access to mandatory training online, to support the development of e-learning and to make compliance visibility much easier for line managers to enable them to support their staff to complete their training.
3.11 Involvement of the Trust’s governors
The Trust’s governors continue to take an extremely valuable and active role in providing the Trust with views and opinions of members and the public and contributing to the planning of future services. During 2022/2023 developments in respect of governors’ involvement include:
- Continuing to engage and deliver the Governor and Membership Strategy to maximise governors’ abilities to comply with their key duties to represent the membership and wider public, and to hold the Board to account via the Non-Executive Directors.
- Listening to members of the Trust and the wider public’s issues and working with Trust officers to provide responses to the issues raised, using the iLog process.
- Inputting into public engagement events in relation to Trust services such as mental health rehabilitation, the temporary closure of the psychiatric intensive care unit, crisis services and child and younger adult services.
- Participating in some 15 Steps quality visits and objectively reviewing services from the perspective of service users and the public.
- Engaging with Trust staff at Chief Executive Officer (CEO) Roadshows and drop-ins across Trust services to engage with staff and broaden their perspective of the services on offer.
- Holding the Board to account for quality standards by receiving regular reports and challenging the Non-Executive Directors for performance results.
- Contributing the views of members and content to the Trust’s strategy and forward plan.
- Contributing to the equality, diversity and inclusiveness work across the Trust including attendance at related conferences and meetings.
- Receiving training and development days regarding the roles and responsibilities of governors to ensure effective performance in the role.
- Contributing to staff and non-executive director recruitment processes.
- Contributing to cost improvement programmes through involvement with quality impact assessment panels.
- Supporting with the facilitation of a governor and membership stall at engagement events for events such as older adult and frailty, college open days and community connector events.
- Participating in Trust focus groups such as Building Together, Autism Strategy task and finish groups and the mental health liaison team meetings to provide comments and feedback on behalf of members and the public.
3.12 Board assurance
The Trust Board is accountable for ensuring all Trust services genuinely and consistently meet the essential compliance standards for quality and safety. The Trust Board ensures it remains well informed and visible across its services. The Board maintains a regularly reviewed Board Assurance Framework (BAF) and receives detailed quality and risk reports. The Committees of the Board each receive assurance reports to enable the content of the BAF to be validated. Board members visit clinical areas and Board members seek additional assurance where there are residual concerns for quality and service user/patient safety. The Board has a robust assurance and escalation process, which ensures its members are promptly informed of any high-risk concerns across services. The Board seeks additional assurance via the use of its committees’ analysis of “deep-dives” into areas of variation.
The Board ensures its accountability for quality and service user/patient safety through mechanisms including the following:
- Setting strategy and policy that is in line with best practice and statutory requirements.
- Ensuring focussed Board time is dedicated to discussion on quality and service user/patient safety issues.
- Receiving assurance reports and leading the effective provision of safeguarding, infection control, mental health and mental capacity act compliance, information governance and environmental enhancements to estate and the carbon-zero targets.
- Effectively monitoring the quality of care provided across all Trust services through critically reviewing internal and external quality and risk reports, including those evidencing benchmarking of the Trust’s services locally and nationally.
- Proactively scrutinising high-level risks to quality and instructing prompt mitigating action if required.
- Challenging poor performance or variation in quality and actively recognising quality improvement.
- Supporting critical reviews of incidents to identify the factors affecting quality and service user/patient safety and learning from those incidents.
- Leading effective partnership working with other health and social care organisations, within both the Lincolnshire System and the East Midlands Mental Health Alliance.
- Role modelling a culture of listening, transparency, visibility and accountability.
- Provide executive sponsorship to all equality, diversity and inclusiveness staff forums and engages in reverse mentoring.
- Actively listening and responding to concerns to ensure early detection of problems, including to allegations of abuse, so reducing the likelihood of serious failings.
- Being accountable for the quality and safety of care provided, so reducing the likelihood of missing early indicators of serious risk.
- Proactively engaging with service users/patients, carers, governors and staff to support good communication from Board level to ward / team level and vice versa.
- Continuing to prioritise hearing service user/patient/carer and staff stories at both the Board and Committee meetings proactively seeking any associated assurance required.
- Ensuring the Trust provides its staff with good and safe working environments, where they are free from discrimination or bullying. The Board remains committed to ensuring all staff have clear job descriptions, with defined expectations and work in environments where they are supported to achieve the very best possible for themselves and those they care for.
- Utilising and adhering to the operating principles within the national quality board’s framework to assess the quality impact of cost improvement plans, ensuring that the service user/patient always comes first.
- Undertaking annual appraisals to ensure Board members remain up to date, supported and well equipped to undertake their role responsibilities in leading the Trust.
- The Board has in place a Board Escalation and Assurance Framework Policy which is underpinned by a number of other governance policies. There is an annual review of the governance arrangements prepared by the Audit Committee and approved by the Board of Directors.
3.13 Trust highlights of the year
New services/key milestones
- The Trust celebrated a decade of community projects in Lincolnshire Managed Care Network. Working in partnership with Lincolnshire County Council, the Trust managed 10 waves of the Managed Care Network before handing over to Shine Lincolnshire for Wave 11.
- The Trust’s newly launched international recruitment programme welcomed the first five arrivals to its inpatient wards.
- Over 200 of our amazing staff joined us at Lincolnshire Showground for the first in-person Nursing & Care Conference since 2019.
- In May, a new chatbot assistant was launched via the steps2change website. It proved to be a welcome addition with almost 1,200 people in Lincolnshire referring themselves to the service in the first two months of the chatbot’s existence.
- LPFT recruited its first traveller community wellbeing link worker role – the first role of its kind in the region. The post visits a number of county sites to forge positive relationships with members of the Traveller community, while listening to their concerns and signposting them to the support they need.
- In July, the Trust launched a new menopause in the workplace guidance as we continue to strive to promote a better understanding and support for employees experiencing the menopause.
- LPFT assumed temporary financial support and oversight of the children and young people counselling service at the Lincolnshire Centre for Grief and Loss (LCGL), after the grant agreement between Lincolnshire County Council and the centre came to a natural end.
- A number of staff were celebrated as the Team LPFT Values Awards returned to being a face-to-face event for the first time since 2019.
- In November, the Trust took the difficult decision to temporarily close the Hartsholme Centre on Long Leys Road in Lincoln, which provides psychiatric intensive care for men.
- In December we launched our QUIT programme. The programme will make effective treatment for tobacco dependency part of the routine care offered to our inpatients. The programme will initially be available to all patients on our adult rehabilitation wards (The Fens, The Wolds, The Vales, Maple Lodge and Francis Willis Unit), before being rolled out in 2023 to all adult inpatient wards.
- In January, an exciting expansion to the Mental Health Support Teams was announced. New teams are set to launch in Spalding and the surrounding area from September 2023, and Grantham and Sleaford from January 2024. These are in addition to existing successful teams in Lincoln, Gainsborough, Boston and Skegness.
- The Trust was successful in receiving additional funding to progress work on the new Boston adult acute inpatient ward, due to be built at Norton Lea in the town. Work is now ongoing to finalise designs and start work on site.
- Work continued and almost completed on the Lincoln Peter Hodgkinson Centre site on the replacement of Conolly and Charlesworth adult acute wards. Due to open in June 2023 the new wards will provide individual ensuite bedrooms and vastly improved ward environment.
- In February 2023, we expanded the psychological support to women and birthing people following the loss of a baby and those who are pregnant again following a loss with the launch of a new perinatal trauma and loss care service.
- Work continued to expand the integrated place-based teams and local community connectors and social prescribers as part of the community mental health transformation programme. As well as expand the network of local Night Light crisis cafes across the county.
- The newly introduced mental health urgent assessment centre was able to extend its access to Lincolnshire Police and service user walk-ins in an expansion of our support to prevent attendance at local A&E departments, as well as provide assessment and care in a more suitable care environment.
- The CYP Access Team, formerly known as the Here4You Access Team celebrated its one-year anniversary in January.
- In January the Trust launched its Perinatal Trauma and Loss Care service, expanding its offer of psychological support to women and birthing people following the loss of a baby and those who are pregnant again following a loss.
- How Are You (H.A.Y) Lincolnshire launched in February – a family of websites that bring together everything in the local community that boosts wellbeing.
- The Trust launched new NHS video call memory assessments to help people over 18 years of age who are having problems with their memory, language or attention.
- In March, the Trust formed an exciting new partnership with Age UK Lincoln & South Lincolnshire to promote a range of research studies.
Awards
- Seven AHP Support Workers received nominations in Health Education England’s (HEE) first ‘Celebrating Inspirational AHP Support Workforce National Webinar’ in December 2022, showcasing the brilliant work of England’s AHP Support Workers. With one of the Trust’s Occupational Therapy Assistant at Peter Hodgkinson Centre announced overall national winner of the ‘Positive, Compassionate and Inclusive Award’.
- The Trust was top shortlist for ‘Changemaker of the Year’ at the 2022 MIDAS Awards (Midlands Inclusivity and Diversity Award Scheme) for work carried out by the Bullying and Harassment Steering group. This is in line with the LPFT value of ‘valuing everybody’ and builds on the Trust’s commitment to providing a workplace where all colleagues feel a true sense of belonging and are safe and protected from the harm caused by discrimination of any kind.
- Our Mental Health Support Teams (MHST) which provide mental health support in over 80 schools in Lincolnshire, won the Together Award at the BBC Make a Difference Awards in September 2022. The teams were selected by the judges for their new ways of working with young people, including creating a podcast covering a range of emotional wellbeing topics.
- Liana Vignoni, one of our Practice Educators, was shortlisted for the Nursing Times Workforce Awards in September 2022. Liana was recognised in the Practice Educator of the Year category, in recognition of the Health Care Support Worker Development Programme she created for staff within the Trust.
- Lincolnshire’s Children and Young People Complex Needs Service was recognised in the 2022 NHS Parliamentary Awards in June, having been announced as the regional champion in the excellence in mental healthcare category. The Children and Young People Complex Needs Service works as an integrated partnership between Lincolnshire Partnership NHS Foundation Trust (LPFT), Lincolnshire County Council (Children Services) and other partner agencies such as education and the criminal justice system, providing holistic support to young people who are at risk of homelessness, criminalisation, or exploitation.
- Francis Willis Unit service users were successful at the Mental Health Safety Improvement Programme Learning Event Awards run by the East Midlands Patient Safety Collaborative (EMAHSN). The patients were nominated for their Patient-led Choice and Responsibility Quality Improvement Project in the category of Co-production Award for Encouraging Outstanding Patient and Public Contribution.
- Jodie Gunson, a Nursing Apprentice at the time and now a registered Nursing Associate, was shortlisted for Nursing Associate Trainee of the Year at the Student Nursing Times Awards. She was also a finalist at the Lincolnshire Apprentice Champion Awards in May 2022.
- Lorena Hall, Medical Student Lived Experience Educator at LPFT, was shortlisted for ‘Positive Role Model Award for Disability’ at the National Diversity Awards. As well as working with People First self-advocacy, Lorena teaches as a lived experience educator in autism and learning disability in local higher education programmes and is also studying a PhD researching health inequalities for people with learning disabilities in Lincolnshire.
Accreditations
- In August 2022, Lincolnshire’s Sexual Assault Referral Centre (SARC) once again achieved the Lime Culture Quality Mark for Independent Sexual Violence Adviser (ISVA) Services.
- LPFT achieved the silver award in the Defence Employer Recognition Scheme (ERS) in July 2022. This was first achieved in 2017 and can be renewed every five years. The award is an acknowledgement of the Trust’s role in supporting members of the military community working in the Trust, particularly within the Veterans Service.
- In March 2022, the Ward 12 team which is an acute adult inpatient service at Boston Pilgrim Hospital, reattained its QNWA (Quality Network for Inpatient Working Age Mental Health Services) accreditation
- Grantham Crisis Resolution and Home Treatment team successfully secured its HTAS (Home Treatment Accreditation Scheme) accreditation again. The accreditation acknowledges the team’s commitment to provide support for people having difficulty with their normal coping methods for mental health issues and working with them to try and care for them in their community to prevent the need for them to go to hospital.
- The Veterans Service and the Trust’s community, inpatient and crisis teams were reaccredited with the Lincolnshire Carers Quality Award, acknowledging the valuable support LPFT provides to carers it works alongside.
- In February 2022, the Trust received a Stonewall Gold Award for our commitment to LGBTQ+ inclusion at work.

