Triangle of Care
What is the Triangle of Care?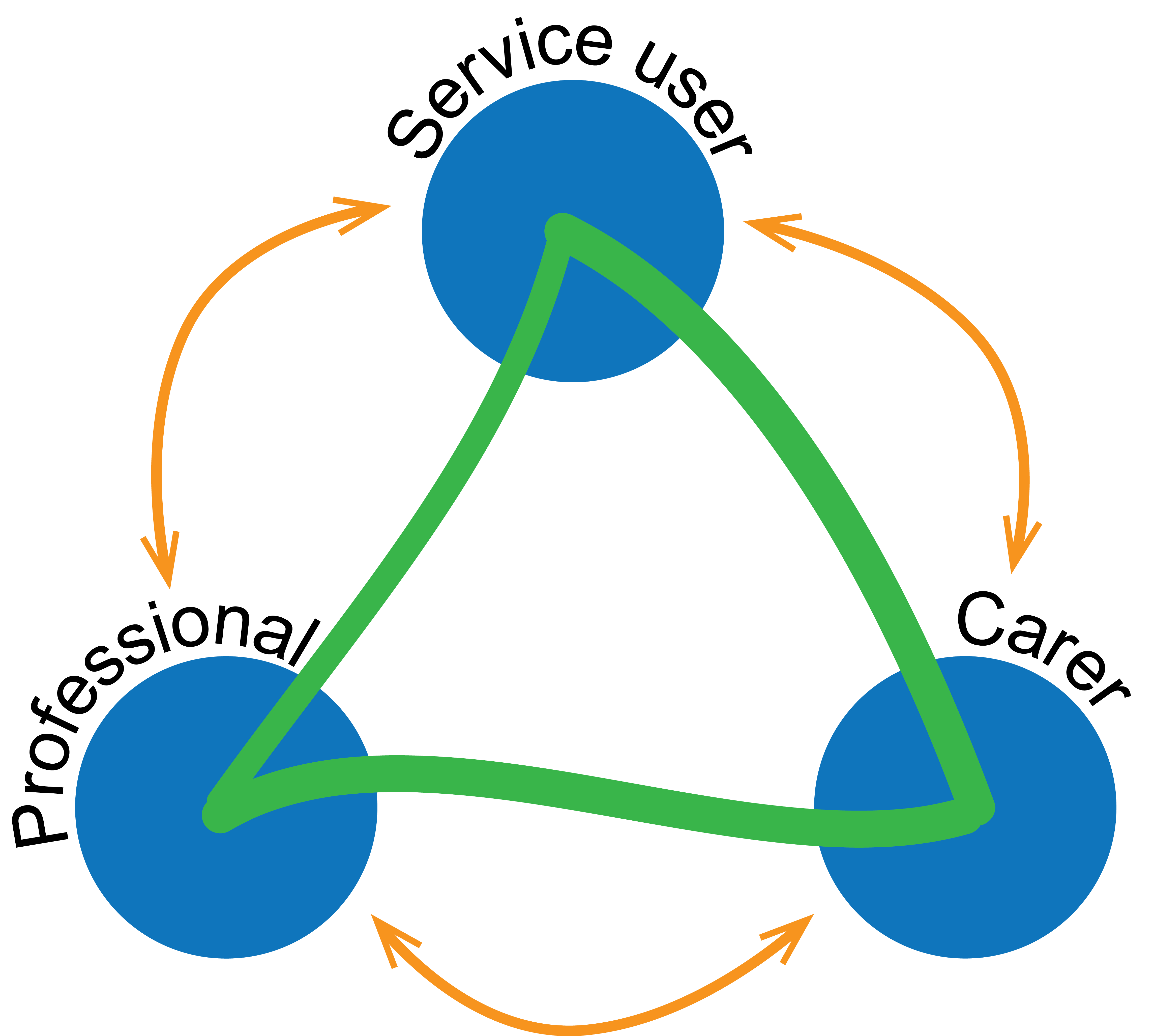
The Carers TRUST developed The Triangle of Care approach to improve Carer and relative engagement. The Triangle of Care is used in all inpatient services and home treatment services.
The Triangle of Care initiative brings together Carers and relatives, service users and professionals. It aims to promote safety, aid recovery and sustain wellbeing of people with mental health issues and their Carers and families.
How the Triangle of Care can help Carers and relatives
As a Carer and relative you may be the only consistent form of support the person you care for has. You are the person who is there when the person you care for is:
- Well
- In need of help with day-to-day activities
- In crisis
You most likely have the wealth of understand of the person's needs and condition. This makes you a vital partner in providing their care. Professionals should recognise the support given by Carers and acknowledge their key role. In doing so, they promote resilience and encouragement for the recovery journey.
A Carer is entitled to a Carers Assessment regardless of their own financial situation, or the level of support they provide. The Carer Assessment is for the benefit of the Carer. It can be completed with or without the presence of the service user.
A Carer can self-refer to the local authority to request a Carers Assessment or ask a professional to make the referral for them. To request a Carers Assessment contact the Customer Service Centre, Lincolnshire County Council on:
- Tel: 01522 782224 (From 8am-6pm, Monday to Friday)
- Tel: 01522 782333 (From 6pm-8am emergency out of hours)
- Email: carersservice
@lincolnshire.gov.uk
Meet The Team
As a Carer you will meet a wide range of staff both in hospital and in the Community. At times their roles overlap and/or you will see them in both hospital and community environments We have listed the staff and their role in the Team.
In Hospital
Chaplain
The chaplaincy and spiritual care team help people to build up their own inner resources. They help people use their spirituality to give themselves greater confidence. They will support any service user regardless of their culture, religious background or beliefs. The chaplaincy team participate in many activities, to promote a greater knowledge and understanding of mental health issues, especially within the wider faith communities. They are supported in their work in the Trust by chaplaincy volunteers. If a Carer, or a service user, wish to speak to a chaplain please ask ward staff to contact them on your behalf.
Carer Lead
All wards and teams within the Trust have a designated Carer Lead. This staff member will have extra training to enable them to fulfil this role. Carer Leads wear an organge lanyard rather than the standard NHS blue. The role of the Carer Lead is to:
- Develop greater awareness of Carers with the team, supporting colleagues to identify and be sensitive to the needs of Carers of all ages
- Promote good pratice and partnership working with Carers by communicating directly with Carers and support them from access meetings to raising concerns
- Develop and maintain systems to identify Carers and provide support
- Ensure that there is relevant and up to date information available for Carers
Consultant Psychiatrist/ Responsible Clinician
Consultants are a medically trained doctor who are specialised and trained in psychiatry. Our consultants are able to discuss, review and prescribe medications. They may also recommend holistic therapies such as dialectical behavioural therapy. Please be aware that a service user may have a different consultant in an outpatient setting to an inpatient setting.
Psychologists
Psychologists work in many different areas of society and are concerned with practical problems. Psychology is the study of how people think and behave, that is a combination of science and practice. They make assessments of a patient's problem by using:
- Direct observation,
- Interviews and
- Techniques such as psychometric testing
Treatment usually takes place over a series of sessions and requires the cooperation of the patient.
Ward Manager/Service Manager
The role of the Ward Manager or Service manager is to ensure a high quality, safe and effective level of care and oversee the day to day running of the Ward or service. The manager is available to talk to if you have any particular questions or concerns that the nursing team cannot answer or resolve for you.
Named Nurse
In an inpatient setting, service users will be allocated a named nurse who will offer one to one support. This contact is important to build a rapport and trust with an individual staff member. The nursing team are able to discuss concerns and to develop a care plan to address any areas which require support or interventions. Nurses will also administer prescribed medications and injections. Named nurses are an important contact for Carers as they are central to communication between the ward team, Carer and patient.
Healthcare Support Workers
Healthcare Support Workers support the role of qualified staff to ensure that service users are being nursed in adherence to their continuing care plan.
Pharmacy
The Pharmacy team are able to provide information and advice on medications. Their role is to help carers and patients to:
- Understand the medication prescribed
- The intended outcome of taking the medication
- The best option available and alternatives
- Any side effects
- How to take medication
The pharmacy team have a wealth of information on the Trust’s website. This has information about conditions as well as the typical medication used to manage symptoms. You can ask the nursing staff to make an appointment with a pharmacist if you wish to speak to someone face to face
Occupational Therapist
The role of occupational therapy is to promote service user’s independence. Occupational therapists may liaise with Carers to get an idea of what interests and level of engagement the service user may have. They complete home visits and assessments, such as cooking, vocational and community skills and offer interventions surrounding this.
Within the therapy team is a chartered Physiotherapist who is able to assess movement and function when someone has an injury illness or disability. They will prescribe interventions such as exercise plans and adaptions/equipment with the occupational therapist.
In the Community
Community Psychiatric Nurse (CPN)
A CPN is a qualified nurse who is based in the community rather than the inpatient setting. The CPN will act as a service user’s key worker and acts to refer the service user to other mental health professionals. The CPN may visit service users at home, at a GP surgery or at the community mental health’s team base.
Service manager
The role of the Service manager is to ensure a high quality, safe and effective level of care and oversee the day to day running of the service. The manager is available to talk to if you have any particular questions or concerns that the nursing team cannot answer or resolve for you.
Care Coordinator
The Care Coordinator conducts a holistic approach to care and ensures that the multidisciplinary team conduct regular reviews (usually six monthly unless otherwise agreed). They provide continuing evaluation and assessment of the service users continuing care plan. The Care Coordinator will coordinate the care when the service user is in the community and will continue to be involved if the service user requires going into hospital for any period.
Lead Professional
The lead professional is the delegated person in the team who will support you and oversee your care and treatment.
Care Programme Approach (CPA)
The CPA identifies:
- The needs of patient through using an assessment process
- A named professional responsible for coordinating care
- A written care plan or statement of care
- A regular review of care
What is a CPA review?
A CPA review is completed on a regular basis regardless of whether the service user is an inpatient or outpatient. This involves relevant professionals, a handover from therapy team and will often request Carers’ presence so that you can relay information to the team. The team will speak with the Carer about the approaches to be taken and discuss any proposed leave from the ward.
A CPA meeting will always be held before a service user’s discharge from mental health services in order to agree an appropriate discharge plan of care. If you cannot attend a meeting please speak to a member of the nursing team or the responsible clinician to express your views.
Crisis and Contingency Planning
For service users that go on leave or are discharged from inpatient services a Crisis and Contingency Plan will be collaboratively developed with service users, carers and nursing staff.
The Crisis and Contingency Plan purpose is to agree the details of how to manage difficult situations which may occur. More information can be found below on how to deal with different situations:
- Crisis & Emergency Planning
- Talking to someone with Delusions, Unusual Beliefs and Hallucinations
- Deal with Difficult Behaviour
- Deal with Self Harm
- Looking after someone with Dementia
Carers rights to confidentiality
The Trust’s policy states that staff should be
“sensitive to the service user’s wishes and confidentiality requirements; engage with family members and carers as care partners”
Further information is provided on our Carers rights to confidential page.
Advance statement/directive
An Advanced Statement is a broad term used to describe a service users wishes about their:
- Continuing care and treatment
- Involvement of an advocate, family member or next of kin
- Personal beliefs and values.
An Advanced Directive is a specific term used in Crisis and Contingency Planning. It describes the preferred treatment choices and strategies.
Advanced Statement/Directive should be discussed and decided after an inpatient admission, when the service user is demonstrating the ability to reflect and has capacity.
The patient must demonstrate capacity at the time of making the statement or decision and this information must be documented appropriately.
An advance statement/ directive is not legally binding but healthcare professionals should take them into account when the service user’s capacity is lost. It is a good idea to discuss these with the person you care for when they are mentally well.
Safeguarding
Mental health professionals have a duty of care to report any information that may indicate that a person is at risk of psychological, physical, emotional, financial abuse and neglect.
Please be aware that any information you, or the service user, share that raises concerns about yourself or someone else may have to be reported to the safeguarding team.
Staff will ensure that they gather as much information as they can, to take to the service manager (if appropriate) and multidisciplinary team.
The team will then discuss whether a safeguarding referral is needed at that time. Staff will ensure, where possible, that any concerns are discussed with you directly and further information will be shared if a safeguarding referral is deemed necessary
Deprivation of Liberty (DOLS), Capacity and Advocacy
Deprivation of Liberty (DOLS)
DOLS can only be applied to informal service users who are deprived of their liberty. This means that restrictions have been placed upon them, which are against their human rights, in order to minimise risk. DOLS can only be applied to service users who do not have capacity.
Capacity
Capacity is the ability to make decisions for yourself about a particular matter. Having capacity means being able to:
- Understand and retain information about the decision
- Understanding the consequences of any choice you make
- Taking that information into account
- Being able to communicate your wishes
Advocacy
TotalVoice Lincolnshire is an independent service that can provide support and information to carers of all LPFT service users.
TotalVoice is also able to signpost Carers to services with regards to financial issues, counselling and mediation.
To contact TotalVoice or telephone 0300 303 1660
Prevention & Management of Violence and Aggression (PMVA)
Within inpatient services it may be necessary to utilise PMVA techniques to prevent harm to self or others.
Nursing staff are trained in various de-escalation techniques, which are always used before any restrictive interventions. The physical holding of patients is always used as a last resort. It is only used when all other interventions have been attempted, or the situation is an emergency and there is a need to administer medication.
If you are witness to any intervention please remove yourself for your own safety. If you are witness to any incident which causes you concern, please seek out a member of staff, once they are free, to discuss your concerns.
Nursing staff will only physically intervene to prevent a service user from harming themselves or other people.
Mental Health Act Section & Community Treatment Orders
Mental Health Act
If a service user is said to be an "Informal", then this means that they are in agreement to stay as an inpatient on the unit to be assessed and receive treatment if required.
If a service user is said to be "Formal", then this means that they have detained under "Section" of the Mental Health Act 1983. The most common "Sections" used are as follows:
- Section 5(2) – Doctor’s holding power for up to 72 hours to allow further assessment
- Section 5(4) – Nurses holding power for up to six hours to allow further assessment.
- Section 2 – Assessment for up to 28 days
- Section 3 – Treatment for up to six months, which can be renewed for a further 6 months, then yearly
- Section 136 – Used in public places, by the police, to take a person to a place of safety for assessment for up to 24 hours. This can sometimes be extended for 12 hours
- Section 135 – Warrant to remove a person from a private dwelling for assessment
- Section 17 – Leave of agreed absence that can be taken from the unit
- Section 37/41 - Hospital order imposed by court with no specified time but will have certain restrictions if the 41 is in place
Community Treatment Orders (CTOs)
CTOs were introduced into legislation for England and Wales by the Mental Health Act (MHA) 2007. They can be applied to a patient who is already subject of the MHA which makes them liable to be detained for treatment.
The Community Treatment Order may mean that a patient is subject to conditions in the community, such as medication. You may be required to take medication prescribed for you by your doctor if you are on a CTO under the Mental Health Act. There are rules in place, called "Consent to Treatment", that cover whether you should take it in the community.
Being in the Ward environment
Locked and Unlocked Wards
Wards may be locked in order to keep informal and formal service users safe. If all service users are detained on a ward the ward can be locked on a permanent basis.
Wards which have a mixture of both formal and informal service users may lock their doors. However, informal service users have a right to leave the premises on request, unless they present as a risk to themselves or others. Informal service users insisting on leaving the premises may be assessed under the Mental Health Act.
Smoking
We do not encourage smoking on any of our Trust sites. If you choose to smoke you must leave our premises. Due to the restrictions on smoking we therefore ask that you do not bring in any lighters, matches or smoking related items onto the premises. E-cigarettes can be used in designated outside areas. Nicotine replacement therapy is available for service users and stop smoking advice is given to service users who request it.
Compliments, suggestions and complaints
We hope that your engagements with LPFT services remain positive and ask that you take the time and opportunity to inform us of any concerns or compliments that occur to you.
Our lessons learnt approach ensures that we listen to our carers and use their comments to shape future care in the best possible way.
Please inform a representative from the appropriate service of any complaints that you may have in order to allow us to immediately address your concerns.
If you are not happy with the results of this meeting then please put your concerns in writing to the service manager (Staff can provide you with the appropriate contact details).
If you feel you do not get a satisfactory answer from the service manager then please contact Patient Advice and Liaison Service (PALS) or telephone on 01529 222265 You can also refer to our Experiences Count page for more information

