Student and new starter information - Witham Court and Langworth Ward
Welcome to Witham Court and Langworth Ward!
A warm welcome to all our new starters and students. The information set out over the page below is designed to help you navigate your first few days. Please do read on to help you find your way around Langworth Ward and the wider Witham Court complex and get an understanding of who we are and what we do.
Staff facilities
Food and drink
There is a staff dining room situated on the main corridor for you to use, please ensure you leave this area as you would like to find it. Unfortunately there is no onsite catering for staff so you will need to bring your own food for which there is a designated fridge in the ward kitchen. There are two supermarkets nearby. Please do ask colleagues for directions if you're unfamiliar with the area.
Smoking area
Please note that the Trust and the site has a no smoking policy. Smoking is not permitted anywhere within the building but there is a designated smoking area just outside the grounds.
Car parking
The car park at Witham Court is free, but can get very busy in the middle of the day. There is a council run car park across the road (no parking charges). Please do not park in disabled bays unless you are entitled to do so.
Toilets
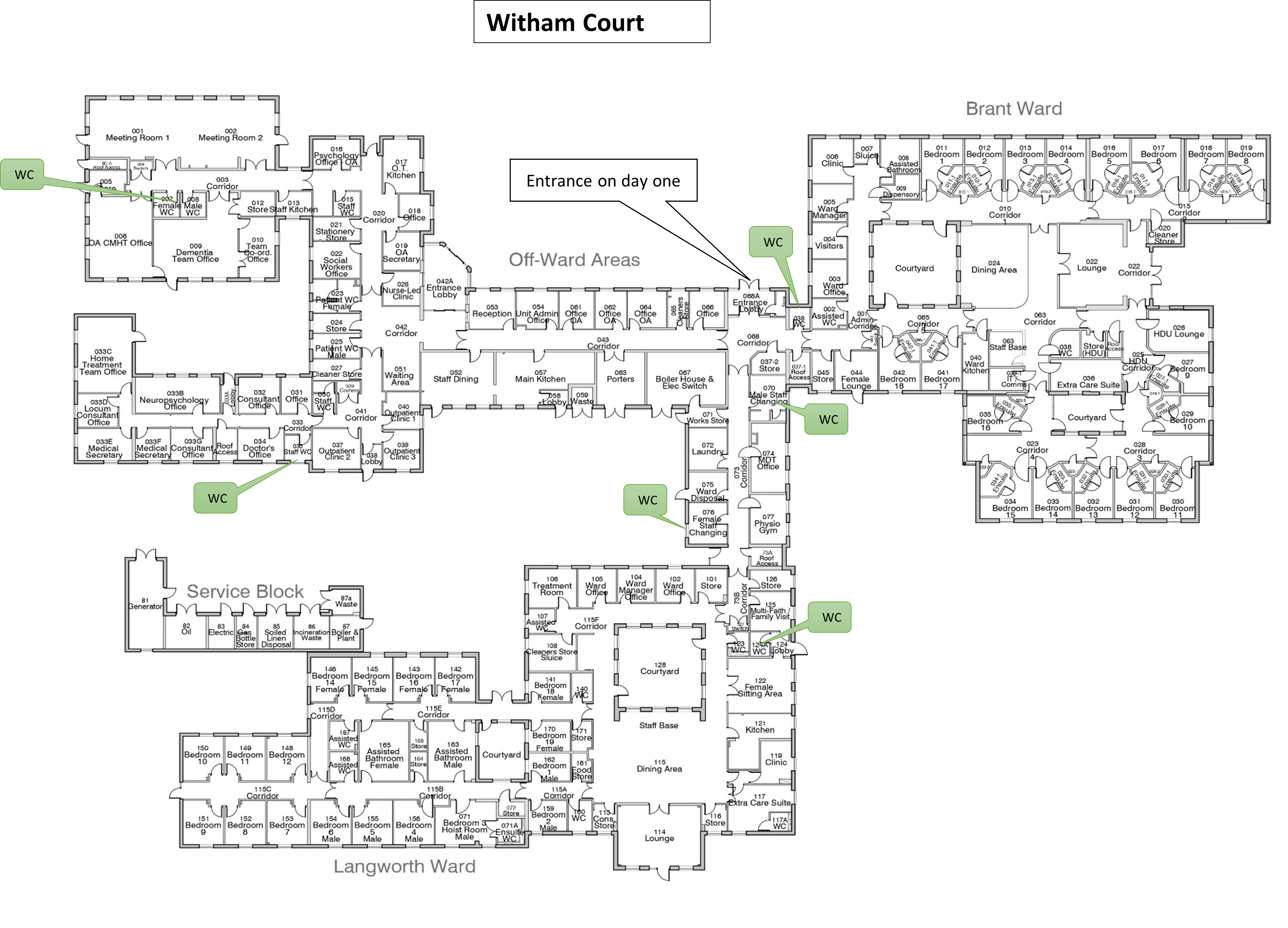
Toilets are marked on the floor plan.
Important information for your shifts
Shifts
We provide a 24 hour service comprised of the following shifts, worked in combination over 75 hours a fortnight. Allocation of shifts will be discussed on day one.
|
|
|
|
Therapy staff work a slightly different shift pattern and do not work at night.
Dress code and infection control
Uniform is worn at all times on the ward and must be laundered daily to minimise the spread of infection. Uniform should not be worn travelling to and from work. Please change in the locker room and lock your property in the lockers provided (you will need a small padlock). Please take everything home at the end of your shift.
Students should wear the tunic provided by the University (if provided). If your student branch only provides polo shirts, please wear that.
Please keep jewellery to a minimum (nothing that dangles as they could be grabbed and pulled). Wedding bands only, no other rings. These measures are taken to minimise the risk of infection transmission and potential accidental injury of patients.
All staff must have bare arms from the elbow down. No watches or cardigans/pullovers when working with patients. This again is to minimise the risk of infection transmission.
Security and building access
Access to the building and various parts of the ward is via access card or a key.
You will be issued a master key and door swipe for the duration of your placement or at the start of your employment. When entering or leaving the building/ward, please ensure you close the door securely behind you as patients may try to follow you.
If someone wishes to enter and you do not recognise them, do not hesitate to ask for identification. If in doubt, advise them to enter through the main entrance at the front of the building where they will be met by reception staff. Close the door securely behind you. Out of normal working hours access, if in doubt of a person's identity do not open the door.
Please report any suspicious activities or security breaches to the nurse in charge. Identification should be worn by all staff whilst on site. Inform the nurse in charge of anyone not wearing identification.
Personal belongings and mobile phones
Please keep personal belongings out of sight in a vacant locker in the staff toilets (you will need a small padlock for this). Please do NOT leave personal belongings in the nursing office.
Mobile phones should not be taken into the clinical area unless you have a specific reason previously arranged with the nurse in charge. Taking pictures of patients is expressly forbidden at all times.
Emergency call system for staff
The unit operates an emergency staff call system activated by individual fobs allocated at the start of each shift or by call buttons located in most patient areas and rooms. It is important that you ensure the fob is returned at the end of the shift to prevent shortages for the oncoming shift and thus not placing them and patients at risk. The purpose and use of these will be explained on your first day.
Telephones
For calls within Witham Court just dial the extension you require. No prefix is required for any external calls. If you experience any problems with your telephone please contact reception.
Photocopier/printer
The photocopier and printer is located in the ward Clerks office, this requires smart card access. If you have any problems with the photocopier/printer please notify admin staff.
IT access
The Trust provides e-mail, web-based services and desktop applications (access dependent on role). IT access will be granted after completion of relevant documentation supplied as part of this induction. It is advisable to read the Trust policy (Computer Use Policy) in relation to the do’s and don’ts as breaking this policy may cause breaches in confidentiality. Students will need to have their access on Rio changed to reflect the placement, staff on the ward can assist in this.
Fire safety
For your safety and that of others, please familiarise yourself with the layout of the premises, fire action notices, your nearest means of escape, where the nearest firefighting equipment is located, and where the nearest break glass point is located.
If you discover a fire;
- Sound the alarm at the nearest call point
- Nurse in charge to dial 999
- Ward staff to report to the nurse in charge for instruction and begin to prepare to evacuate staff from the fire locality (remember to keep at least 2 fire doors between patients and the fire)
- If advised to evacuate, do so using fire exits as instructed
- Non-ward staff to proceed immediately to the nearest fire exit and leave the building
- Walk… Do NOT run
- Do not stop to collect any personal belongings
- Do not attempt to fight the fire UNLESS it is blocking your exit route
- Meet at the assembly point (Secondary Car Park) and report to the senior nurse to confirm you are safe
- Do NOT re-enter the building until you are told it is safe to do so
Health and Safety
Under Section 7 of the Health and Safety at Work etc. Act 1974 (HASWA), YOU have to take care of yourself and others in the actions that you do, or do not do, whilst at work. This means that if you see a hazard and ignore it resulting in an injury, you will be in breach of this section of the Act.
- You must co-operate with the Trust on health and safety issues, and policies and procedures, and report any hazards.
- You must not interfere with or misuse anything provided for your health, safety and welfare.
- Should you find any hazards within your workplace area or anywhere in Witham Court, please report them to the nurse in charge in the first instance.
Confidentiality Statement
"By law, everyone working for or on behalf of the NHS or other qualified health care providers must respect your confidentiality and keep your information secure”
Your information and health records: Lincolnshire Partnership NHS Trust (lpft.nhs.uk)
Team constituents:
Admin – Two ward clerks, a medical secretary assists with ward rounds currently comprise the administration team.
Nursing – see section below
Medical – medical responsibilities for older persons services in the South West sector are held by a Consultant Psychiatrist, supported by junior doctors on rotation, both are based within Witham Court.
Housekeeping – Housekeeping duties include the preparation of breakfast, lunch and supper ready for the nursing staff to serve to the patients and they are responsible for the cleaning of all areas of the ward including bathrooms and bedrooms and the removal of all waste bags. The Porters duties are re-stocking of the ward linen cupboard, bringing deliveries and post to the ward, doing any minor repairs and any driving jobs that maybe required.
Others – Based in another part of the centre, the South West CMHT works in close relationships with the centre. This includes Community psychiatric nurses (CPNs), Dementia Home Treatment Teams (DHTT), Home Treatment Teams (HTT), social workers (SW) and community care-officers (CCOs)
Client Group
Gender – The unit provides services for up to 9 male and 9 female patients.
Age Group - Older adults (+ 65 years). Occasionally we do cater for under 65s with organic disorders.
Specific areas of identified need – Patients in acute need of detailed assessment and treatment of mental health status that cannot be provided within a less restrictive environment.
Partnerships with other service providers
Clinically the unit works in collaboration with occupational therapy, community mental-health teams (CMHT), psychology, chiropody, infection control, physiotherapy, dieticians, speech and language therapists and general medical services in the delivery of services. Extensive interactions with private care-providers also constitute an ongoing service relationship (residential and nursing care, day-care services, home-help). Further, voluntary agency input to the unit also represents an ongoing collaborative venture. Insight visits with many of these team members are negotiable.
Model of care
The care approach used at Witham Court and Langworth Ward is an adaptation model of nursing - wherein each person is seen and assessed as an integrated whole, with biological, psychological and social components and in constant interaction with the surrounding environment. Here, outcomes related to achieving adaptive responses predominate.
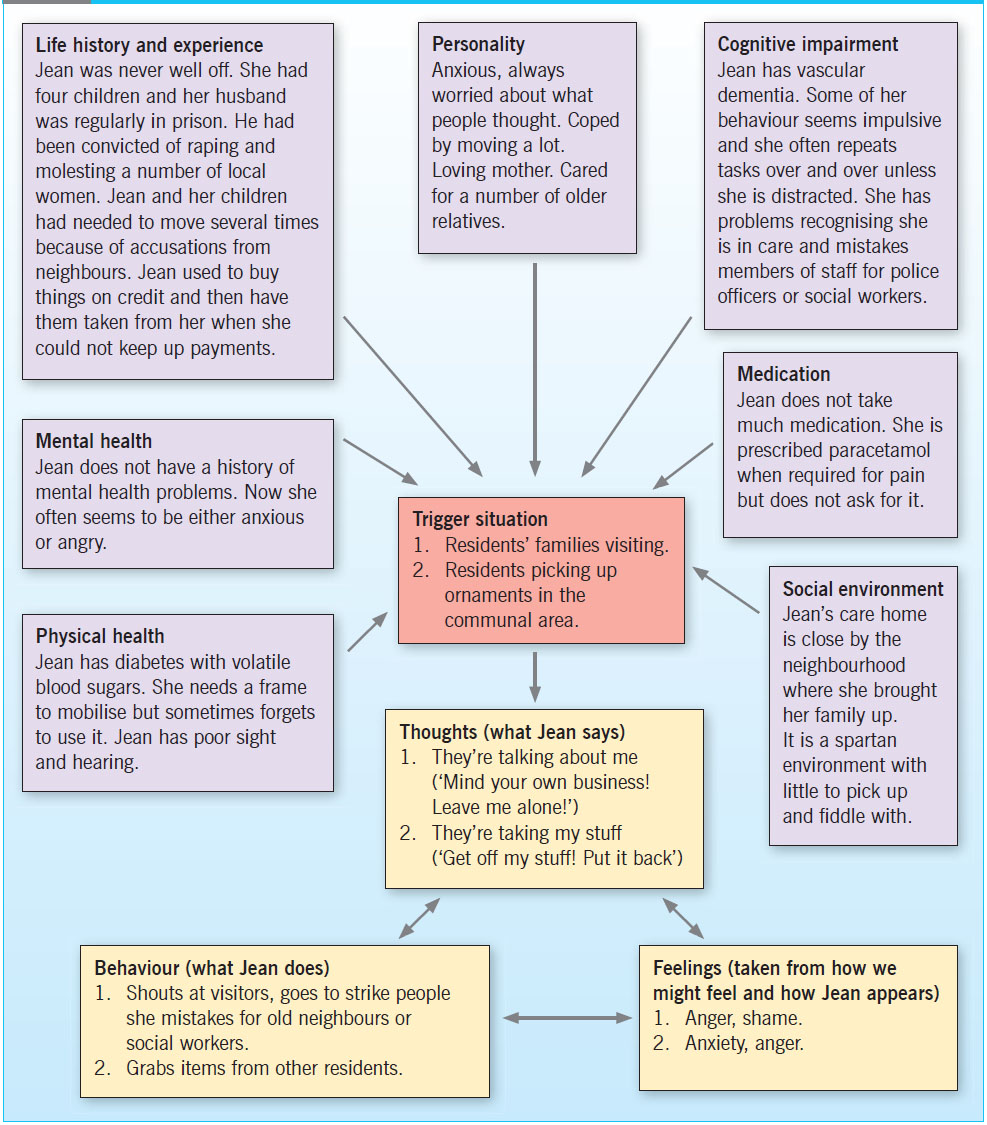
Although we are moving towards an adapted (condensed) version of the Newcastle model that provides a framework and process in which to understand behaviour that challenges in terms of needs which are unmet, and suggests a structure in which to develop effective interventions that keep people with dementia central to their care.
Specific interventions in use:
- Person-centred therapy
- Psychosocial strategies
- Problem solving strategies
- Anxiety management
- Psychopharmacology
An illustration of the Newcastle Model to understand people whose behaviour challenges in dementia care.
John's Campaign and Triangle of Care
Please familiarise yourself with our adopted approach to ensure inclusion of carers.
John's campaign
 John's Campaign has a single, simple message: no one should enforce disconnection between family carers and those who need their expert knowledge and their love. This principle is applicable everywhere: in the doctor's surgery, the A&E ward, the dementia assessment unit and the care home.
John's Campaign has a single, simple message: no one should enforce disconnection between family carers and those who need their expert knowledge and their love. This principle is applicable everywhere: in the doctor's surgery, the A&E ward, the dementia assessment unit and the care home.
Families are never “visitors” to a person with dementia; they are an integral part of that person's life and identity and often their last, best means of connection with the world.
Lincolnshire Partnership NHS Foundation Trust is a participant, along with over 1500 hospitals and homes (and some others, such as ambulance trusts, clinical commissioning participants, domiciliary care companies, hospices and primary care providers) and has pledged to support the principles of inclusion. We believe that people, particularly those with dementia, other mental illnesses, or otherwise in need of care, should not be separated from those important to them by protocols and systems that are harmful and wrong.
Triangle of Care

The Trust is accredited by the Triangle of Care, an initiative which brings together service users, carers and professionals aiming to promote safety and recovery for people with mental health issues and to encourage their wellbeing by including and supporting their carers. The ward has a number of Carer Ambassadors who promote inclusion, involvement and our support of carers amongst all ward staff. Our Carer Ambassadors will be wearing orange lanyards or badges to help you identify them. Do take the opportunity to talk to them about how you can get behind this initiative too.
Nursing and clinical staff
Nursing
The nursing team is comprised of a unit manager supported by Ward Sister/Charge Nurses. The management team supports a team of staff nurses and nursing assistants.
Band 7 Manager Role
Band 7 Practice Development Nurse role
Amelia
 About me and my role
About me and my role
- I am a Registered Mental Health Nurse
- I have been working on Langworth Ward since 2017.
- I am part of the Leadership Team for Langworth Ward alongside Ken (Ward Manager) and Tash (OT Lead).
- I work long days, sometimes this is a NIC, other days this is office based.
- I work with the ACP to implement outcomes from ward round.
- Provide Clinical Supervision and Clinical Development.
- Provide extensive clinical advice and support and enhance the knowledge base and practical skills of the team.
- Development and delivery of formal and informal education and training for staff.
- Attend strategic and developmental meetings.
I can support with...
- Questions around a patients care and treatment.
- Questions and support around our pathway and Dementia.
- Support, guidance and training around assessments, care plans, risk assessment, datix etc.
- Information around nonpharmacological interventions and NICE guidelines for prescribing in Dementia.
- Support and guidance with de-escalation techniques.
- Clinical supervision, reflective practice and debriefs.
- Support and guidance for difficult conversations with family.
- Staffing levels in the absence of the Ward Manager or Deputy Ward Manager.
- Feedback from development and strategy meetings.
Band 6 Senior Acute Care Nurse
Sophie (Soph)
About me and my role
I qualified as a registered Mental Health Nurse in 2020 and have worked on Langworth Ward ever since! I am part of the senior nurses team specialising in the clinical aspect of patient care. I participate in weekly ward rounds to ensure that the nursing and medical team work together efficiently and the care provided is outstanding. I also do clinical and managerial supervisions and support other nurses and health care support workers. So feel free to chat if you need.
I work 3 long days a week and these are the same every week. Some days I will have a ward day where I will be involved in patient care and ‘on the floor’ other days I may have a management day where I spend time doing audits and catching up on paperwork!
You will often see me working with other nurses to ensure that the outcomes from ward rounds are completed. I also spend a lot of time talking and fretting about risk assessments. I am also named nurse to a few patients and therefore will focus on their care plans and risks before others, but happy to help where needed.
I can support with...
I am happy to answer any questions regarding patients, their care and in patient journeys. I can give support on the dementia pathway and the procedures that go with this. I will give guidance in care planning, assessments, risk taking, admissions/discharges, MHA, medications and ward rounds as well as support new nurses through their preceptorship.
We can look at de-escalation techniques if you find this challenging and have discussions in supervision. I can support with personal and team de-briefing and reflections as well as guiding nurses through revalidation.
I can assist with processes and leading meetings and I can support where difficult conversations are needed.
I am happy to help with anything at all, if I do not know the answer to a question, I will do my best to find the answer and we can develop together.
Band 5 staff Nurse role
Band 3 Healthcare Support Worker role
Consultant Clinical Psychologist (Acute Pathways)
Stephanie
About me and my role
- I qualified as a Clinical Psychologist in 2012.
- Working with older people is my passion including those with mental health difficulties, and with dementia.
- I work across Langworth Ward, Brant Ward, and the Home Treatment Teams.
- I have a particular interest in applying principles of trauma informed care across all the work we do.
- I am passionate about advocating for our patients so we hear their voice and understand their perspective/experiences.
- I enjoy delivering training and seeing staff develop their skills and confidence.
- I contribute to service development in the Division and attend management meetings.
- I like buying books but don’t always get round to reading them! I love holidays and exploring new places.
I can support with...
- Assist the team to understand a patient’s presentation and how to support that patient.
- Assist the team to think about possible needs contributing to a patient’s behaviour and how we can meet those needs.
- Facilitate formulation discussions.
- Contribute to discussions in Ward Rounds and CPAs to provide a psychological perspective.
- Assist with using non-pharmacological approaches to support people with dementia.
- Provide training for the team on a range of topics including: formulation, supporting people at times of distress, trauma informed care, Teepa Snow dementia techniques, compassionate care, staff wellbeing.
- Provide clinical supervision.
- Facilitate reflective spaces.
Advanced Clinical Practitioner
Debbie Blant
 About me and my role
About me and my role
- I am a RNMH by background.
- I have worked in the division since 2003.
- Since qualifying as an ACP, I work across the Dementia pathway - Langworth Ward and DHTT.
- I work alongside the consultants and MDT in holistic review and I am responsible for the non-complex patients (ward round).
- I feed into improvement of core assessment processes, capacity, medication reviews, risk assessment, prescribing/de-prescribing and discharge processes.
- Bed management and DHTT patient assessment.
- Liaison with GPs and care homes.
- Assessment of patients / ReSPECT.
- Education, pathway development, research and CQI.
- System networking.
I can support with...
- Advice around assessment and treatment pathways.
- Questions around pathway transition points.
- Prescribing and medication issues.
- Advice on research / evidence-based guidance.
- Non-pharmacological interventions.
- Advice on communication strategies.
- ABC monitoring and trigger identification.
- In-house training and education.
- Clinical supervision.
- Action learning sets.
- Patient examination.
- ReSPECT conversations and escalation
- Ordering TTOs / FP10s.
- Audit.
- Continuous Quality Improvement projects.
Lead Nurse for Carers. Carer, Relative Engagement and Development Lead - OPFD
Lesley Hutton
 Lesley.
Lesley.
Carers Workshop for LPFT/OPFD staff every Friday, 10am-12.30pm - drop me a message and I will support you with an invite and explore carers, confidentiality and carer awareness.
About me and my role
I have been with LPFT since 1994 in many roles throughout my career. Coming to OPFD in 2019. My Role sits across the Older Adult and Frailty Division supporting Carers. We have a small team and support the Dementia Pathway and the Mental Health Pathway. We cover Inpatient and Home treatment, and I also support the Community and other services within OPFD that may have carers who need some or further support. I also support the Carers Education Group, OPFD Stakeholder Forums, and Carers Council, upholding the values of LPFT and supporting the National Triangle of Care and other stakeholder groups supported by PCN, ICB/ICS. and other services that are aligned to the Caring role within Lincolnshire.
As a professional and registered Nurse, I take pride in upholding the NMC Code of Conduct. I enjoy teaching, supporting and educating those that I work with. I also keep up to date with Evidence-Based Practice and Learning. I see myself as leading by example and supporting this by offering pragmatic and supportive leadership and clinical competency and I do this by offering Clinical Supervision, Peer supervision and Debriefs.
I want to enhance the experience that Carers have within our service, especially the ward and show how the team on Langworth Ward deliver and supports Carer's views, ReSPECT Care Planning, advanced care planning and person-centred care. I have undertaken advanced training in Dementia, suicide, and end-of-life care and Post Graduate Training in Mental Health.
Carer peer support worker
Kelly Dealtry
 About me and my role
About me and my role
- I am a mum of 4 children.
- I used to be a supply teacher in early years, I joined the Trust in September 2023.
- I received a higher education in Psychology and counselling.
- I am a mental health first aider.
- I am a Wellbeing champion.
- I work from home and within Witham Court/Langworth Ward.
- I am a carer for my grandfather with mixed dementia which gives me great insight and understanding with carers.
How my role supports...
- Supports carers/family members on admission.
- Weekly calls to families of the impatient to support and advocate for them within MDT.
- Support the staff with communicating with carers/family.
- Organise/ attend coffee mornings/afternoons.
- Accompany carers with visits on the ward if needed.
- Complete carer feedback forms on discharge.
- Complete carer questionnaire on Rio.
- Also having the caseload of DHTT to support and communicate their concerns/worries/struggles.
- If needed, I also support EOL care and support for families.
Pharmacy
LPFT acquires its medication supplies from outside of the Trust via a contract with the Co-op. this is facilitated by a pharmacist who is a Trust employee, supported technicians who do the day to day stock control and ordering.
The pharmacist is involved in the patient care meetings and advises on treatment plans derived by the team. All are approachable regarding medication and management of same.
(Further reading in the appendices)
Physical Healthcare Specialist
Why should we support our patients’ physical healthcare? Seminal publications by Rethink (2012) “20 Years Too Soon,” and MENCAP (2012) “Death by Indifference” highlighted the disparity between the life expectancy of the general population and those adults who live with serious mental illness (SMI) and Learning Disabilities (LD). Due to multi-factorial reasons adults who experience SMI are at a significantly higher risk of developing and dying from preventable chronic conditions such as diabetes and cardiovascular disease. Untreated physical illness in people with mental health problems also places a major burden on health systems by increasing use of unplanned and urgent health care.
Evidence shows that people with a serious mental Illness (SMI) die up to 20 years earlier than the average population in the United Kingdom (Rethink, 2012) and people with a learning disability (LD) die up to 46 years earlier (LeDeR, 2018). The early death of people with a SMI and LD is frequently the result of poor physical health. For example the Mental Health Task Force, 2016 state that 2 out of 3 early deaths of people with a SMI are attributable to physical health conditions such as cardiovascular disease, diabetes, respiratory diseases and cancers.
Involvement with LPFT services in the community and admission to a ward is an invaluable opportunity to monitor the physical health of people in order to make appropriate interventions, improving their quality of life and SAVING LIVES. In order to achieve this we need to focus on the health of the individual as whole (including both physical and mental health) and staff members should be competent and confident in providing physical healthcare. They also should be able to recognise a deteriorating patient, intervening and escalating concerns in a safe and timely manner through appropriate physical surveillance and monitoring. Further to this staff also have an important role in promoting good health with equal emphasis on the mental and physical wellbeing of our service users. Please contact the Physical Healthcare Team should you wish to discuss this further.
Others
Based in another part of the centre, the South West CMHT works closely with the centre. This includes Community Psychiatric Nurses (CPNs), Dementia Home Treatment Teams (DHTT), Home Treatment Teams (HTT), social workers (SW) and community care-officers (CCOs).
Therapy Teams
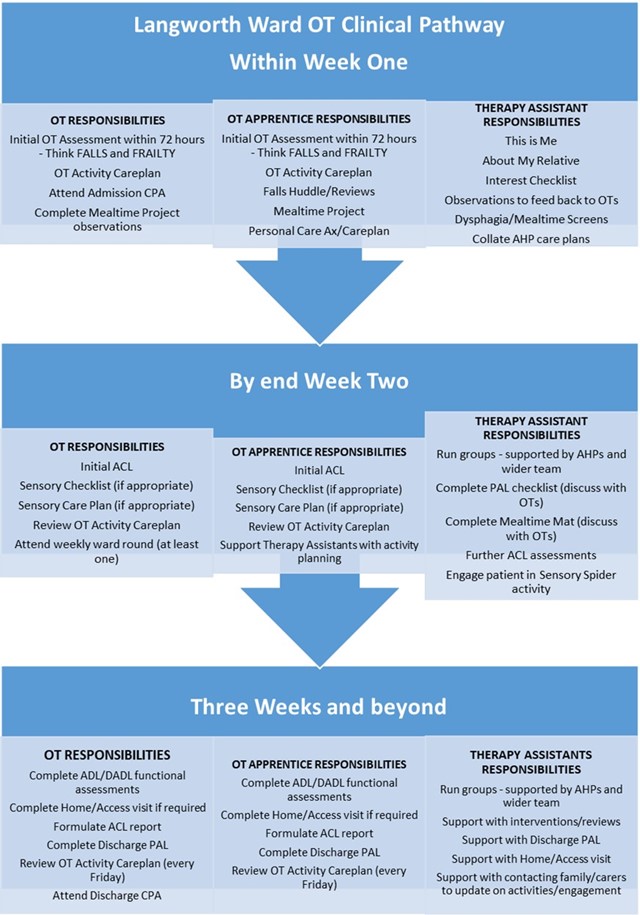
Therapy Pathway 2024

Our North Star Goal
“To provide an enriching person-centred therapeutic environment that enables our patients to feel valued and to live their best day”
(created by Langworth Ward Therapy Team at first Development Day, April 2023)
|
Staff Name |
Role |
|
Natasha Laming |
B7 Clinical Lead OT Dementia Pathway |
|
Carol Rogers |
B5 OT |
|
Gabriella Armstrong |
B4 OT Apprentice |
|
Rachel Johnson |
B4 OT Apprentice |
|
Vivienne McConnon |
B3 Therapy Assistant |
|
Carol-Anne Carter |
B3 Therapy Assistant |
|
Anita Laskey |
B3 Activity Co-ordinator |
Langworth Ward Therapy Team
Langworth Ward Therapy Team is led by occupational therapists and the pathway has been formulated around the Cognitive Disability Model (Claudia Allen 2018). At the heart of our therapeutic interventions is to provide an environment that is truly person-centred, that supports the person living with dementia to have a sense of autonomy and control and to feel that they are at the centre of decision-making.
On the ward we work with people experiencing different levels of dementia. Universally dementia is often described using three different stages; mild, moderate and severe. Occupational therapist Jackie Pool helped to adapt this biomedical approach into a more functional and occupational representation of a person’s ability. Known as the Pool Activity Level (PAL), Pool created four levels ‘Planned, Exploratory, Sensory and Reflex’. The PAL was strongly influenced by Claudia Allen’s CDM. Below is a brief description of the levels. The majority of patients on Langworth Ward are at Exploratory and Sensory level.
Planned Level (ACDM score 5.0-5.8)
The person can work towards completing an activity but not be able to solve any problems that arise while in the process.
Exploratory Level (ACDM score 3.5-4.8)
The person can carry out very familiar activities in familiar surroundings. They will find objects needed to complete task only if they are in line of vision.
Sensory Level (ACDM score 2.0-3.4)
The person may not have many thoughts or ideas about carrying out an activity and is mainly concerned with sensation and moving their body in response to those sensations.
Reflex Level (ACDM score 0.8-1.8)
The person may not be aware of the surrounding environment or even their own body, and may be living in a subliminal or sub-conscious state where movement is a reflex response to a stimulus.
Creating a Therapeutic Environment
We understand the importance of meaningful activity to helping to promote psychological wellbeing and safety to our patients on Langworth Ward. To support this, it is essential for us to work with patients and their care givers to help us build a therapeutic relationship, and to target activities that can engage and stimulate and create a person-centred environment that provides:
- Respect
- Non-judgement acceptance
- Security
- Belonging
- Continuity
- Purpose
- Achievement
- Significance
When someone is admitted to Langworth ward they are encouraged to complete the ‘This is Me’ document with our therapy assistants, and their care givers are offered the ‘About My Relative’ document. These two documents combined can provide vital information about the patient to support us in providing truly person-centred care.
As we build an understanding of the person we are working with, we can begin to create a therapy care plan around that person’s occupational needs. From there, our therapy team will offer a variety of non-pharmacological interventions that may be either cognitively stimulation or rehabilitation-based, and can be utilised as primary interventions to support people living with dementia.
Cognitive Stimulation Therapy (CST)
Cognitive Stimulation Therapy (CST) is an evidence-based intervention that can help promote quality of life and is recommended by NICE (2018).
Within LPFT, prior to the Covid pandemic, CST groups were being run in Older Adult CMHTs providing 12 weeks of group interventions to newly diagnosed people living with mild to moderate dementia.
There groups were stopped during the pandemic and have not restarted. On our inpatient dementia ward, we are able to provide 1:1 and group aspects of the programme within our activity schedule.
The aim of providing CST to our patients is to engage all senses in a range of meaningful activities that systematically target the main cognitive functions including thinking, reasoning, perception and judgement.
CST is appropriate for patients who are identified at PLANNED, EXPLORATORY and SENSORY level.
Cognitive Rehabilitation Therapy (CRT)
Cognitive Rehabilitation Therapy (CRT) involves individualised interventions that focus on specific skills training and practice to support people to maintain skills of every day living.
Where skills cannot be relearned, new compensatory ways of completing them are taught to replace lost cognitive functions.
Compensatory strategies include:
- Grading/simplifying activity ie cooking ready meal instead of making food from scratch
- Using visual memory aids to initial task
- Creating supportive environment ie ensuring items are in eyesight and can easily be found and identified (labelling toothpaste, shampoo, Fixadent)
- Improving environment to reduce auditory/visual figure-ground discrimination problems ie reducing patterns/clutter, turning off TV/radio
Restorative strategies include:
Errorless learning and Effortful processing
- Grading the activity and practising it one step at a time.
- Modelling each step for patient to practice through visual and verbal prompts.
- Gradual reduction in prompts/cues as confidence/competence increases
Unlike CST, CRT is goal driven and therefore is more appropriate for patients who are identified as being at PLANNED or EXPLORATORY level.
Examples of CST and CRT interventions provided on Langworth Ward include:
|
Cognitive Stimulation Therapy |
Cognitive Rehabilitation Therapy |
|
Musical Activities:
|
Practising *PADLs
|
|
Current Affairs Discussion:
|
Practising *DADLs
|
|
Number/Word Games
|
Quizzes/Crosswords/Mnemonics
|
|
Creative Activities:
|
Sensory Activities:
|
|
Sensory Activities: Touch – salt dough shaping, rummage boxes, Busy Bags (see Therapy Newsletter), gardening, massage Smell – cooking, tea tasting, gardening Taste – cooking, tea tasting, meal times Hearing – musical activities Sight – creative activities, observing imaginative art, gardening Doll therapy, Magic Table, Folding laundry, bath |
Maintaining links with community:
|
|
Drama Activities:
|
Reality Orientation
|
|
Spiritual Activities:
|
Spiritual Activities:
|
*PADL – Personal Activities of Daily Living; DADL – Domestic Activities of Daily Living
Behaviours and Psychological Symptoms of Dementia (BPSD)
Working as part of a MDT on Langworth Ward where we work closely with our medical colleagues, supporting the ward with non-pharmacological interventions to support people who are experiencing Behaviours and Psychological Symptoms of Dementia (BPSD) is an important part of our role as a therapy team.
Our interventions include the following:
Understanding the Person
- Information is gathered on admission to identify any known triggers or unmet needs that can indicate when someone is becoming distressed or agitated ie: hunger, thirst, pain, constipation, fear, sensory dysregulation, boredom, immobility
- Background information reaching back to childhood, with details on significant others
- Hobbies, interests and previous occupations
- Past medical history, current functional ability with ADLs etc
Sensory Modulation
Initially the first two weeks of admission are observational from a therapy assessment position, however if there are obvious signs of sensory dysregulation we will follow our Sensory Pathway, based on Sensory Modulation in Dementia Care (Champagne 2011), to support the wider team with care planning to best support the patient. Interventions may include:
- Completing sensory profile with care giver
- Completing Sensory Spider with patient based on information provided by sensory profile on the following: visual, auditory, gustatory, tactile, olfactory, vestibular, interoceptive and propriceptive senses
Positive non-verbal communication
When someone is exhibited signs of BPSD’s which are escalating, they are usually trying to communicate an unmet need that is not being recognised and is causing increasing distress to that person. As their distress increases, they may exhibit behaviours which are challenging to those around them. It is our responsible as care providers to support the person in helping them to communicate their needs in a positive non-verbal way. This can be achieved by the following:
- Active listening, maintaining strong eye contact
- Maintaining an open, welcoming posture and friendly expression
- Communicating clear emotions ie our facial expressions mirroring our words
- Mirroring language used to communicate that we are listening and to encourage further discussion
- Visual prompts and cues i.e. via dementia-friendly pictures or signing
- Approaching the person from the front, not the side, and walking towards them
Reality Orientation
When someone is very disorientated to time, place and person they can feel very threatened by their environment. We can support the person by utilising the following strategies:
- Personalising their bedroom so that they can be gently reorientated during night when it is dark ie provide them with a blanket from home that has a familiar smell, show them photos on the wall of family, show them time on clock
- Discuss time, place and season with the person in a conversational way i.e. do you think it’s warm for summer? It’s nearly the weekend – what do you normally do on a Friday night? Have you ever been to North Hykeham before?
Quality Improvement Projects on Langworth Ward
Mealtime Project
On joining the team in October 2022, I inherited the Mealtime Project which had been started the previous year by Carol Rogers OT, in conjunction with the PMVA Team, with the goal of finding a therapeutic way of helping to reduce incidents of restraint around mealtimes.
The project saw the development of a shift in cultural attitudes around lunch times on the ward, in which all members of our staff, from housekeepers to nurses to HCSW’s could all be involved in creating a therapeutic rather than view it as a routine task.
The environment is adapted to cater to patients according to their PAL level, encouraging those at Planned and Exploratory to sit together, to be more independent with choosing their own food, pouring their drinks etc, whilst those at Sensory level would be provided with increased support, with a visual choice of dishes on offer to alert their senses and trigger a hunger response to maintain good nutrition and hydration (see Resources for more information).
The project is now closed however Carol Rogers is tasked with managing a working group of key stakeholders including patients, staff and care givers to ensure processes are maintained.
References
Allen, C.K. (2018). Allen App: the Allen Cognitive Disability Model (1st digital ed.). ACDMweb. https://
Champagne, T. (2011). Sensory Modulation in Dementia Care.
Pool, J. (2019). Reducing the Symptoms of Alzheimer’s Disease and Other Dementias; A Guide to Personal Cognitive Rehabilitation Techniques
Pool, J. (-). The Pool Activity Level (PAL) Instrument for Occupational Profiling; A Practical Resource for Carers of People with Cognitive Impairment, Fourth Edition: PAL Checklist (qcs.co.uk)
Maclean, F. et al (2022): Occupational Therapy and Dementia; Promoting Inclusion, Rights and Opportunities for People Living with Dementia
Snow, T. Homepage - Positive Approach to Care (teepasnow.com)
Physiotherapy
Physiotherapists in mental health contribute to the multidisciplinary team and inter-professional care. Physiotherapy in mental health is based on the available scientific and best clinical evidence and provide services that develop, maintain and restore people’s maximum movement and functional ability. They can help people at any stage of life, when movement and function are threatened by ageing, injury, diseases, disorders, conditions or environmental factors.
Physiotherapists help people maximise a person’s quality of life, looking at physical, psychological, emotional and social wellbeing. They work in the health spheres of promotion, prevention, treatment/intervention, and rehabilitation. In this trust they also have a key role in the prevention and management of falls alongside the MDT.
Physiotherapists are qualified and registered with the HCPC and are professionally required to:
* Undertake a comprehensive examination/assessment of the service user or needs of a service user group;
* Make recommendations for self-management.
* Determine the outcomes of any interventions/treatments;
* Implement a physiotherapist intervention/treatment programme;
* Provide consultation within their expertise and determine when service users need to be referred to another healthcare professional;
* Formulate a diagnosis, prognosis and plan;
* Evaluate the findings from the examination/assessment to make clinical judgments regarding service users
Student specific information
Please find below information tailored to students but which may prove beneficial reading for all.
Educational Statement:
To provide a supportive student-centred environment, which promotes an integrative approach to the application of theory to practice, in order to facilitate the process of practice-based learning and the acquisition of professional capabilities that lay the foundation for career-long professional development and lifelong learning. Further to this, to support the student in the development of best professional practice and the maintenance of professional standards. To provide and facilitate strategies and methods of teaching that complement the student’s individual learning outcomes associated with contemporary educational programmes and need.
Learning outcomes achievable and opportunities available:
- Core knowledge pertaining to
- Client group – care of older people represents a heterogeneous and complex client area and this is reflected in the breadth of core knowledge. This encompasses but is not limited to a core understanding/awareness of;
- Local and National policies and guidelines driving/influencing change in older persons services (e.g., NSF for older adults, Clinical Governance)
- An understanding and awareness of relevant legislation, policy and procedures and their associated effects upon practice.
- Psychiatric conditions of depression, anxiety and psychotic states, specifically as they relate to older adults.
- Dementing illnesses (types and presentation)
- Influences of chronobiological factors such as altered anatomy and physiology and co-morbid physical states.
- Sociological and psychological influences (e.g. ageism, stereotyping and paternalism) in care-practices.
- Core competencies attainable
- The development of an understanding of the role of the mental health nurse / Occupational Therapist within the specialist care setting.
- The development of therapeutic relationships through the use of appropriate communication strategies and interpersonal skills.
- Active encouragement and participation in appropriate health promotion opportunities.
- The undertaking of comprehensive, systematic and accurate nursing assessment, planning and evaluation.
- The application of evidence-based practice to ensure safe and effective nursing care.
- The acquisition of generic and enabling skills (e.g. effective communication, team working, problem solving and critical reasoning)
- The development of transferable skills relating to the delivery of individual fundamental patient care needs (e.g. medication administration/wound-care/nursing of specific physical conditions/management of anxiety and/or aggression).
- The development of effective inter-professional working practices.
- The development of management skills (personal/professional).
- The continuation of professional and personal development.
- Specific competencies attainable
- Due to the nature of mental health problems within older adults, the placement offers a unique opportunity to explore and develop skills pertaining to;
- The assessment of problems emerging due to brain injury and disease.
- The application and interpretation of specialist cognitive, behavioural and functional assessment tools and pathways.
- Due to the nature of mental health problems within older adults, the placement offers a unique opportunity to explore and develop skills pertaining to;
- Role & responsibilities of Supervisor / Assessor:
The role of the supervisor is a combination of role modelling, supervising, supporting and teaching. It forms a critical element in ensuring that the student gains the maximum from the learning experiences on offer. The role and responsibilities of the Mentor in practice are to;
-
- To support the student during the placement.
- Supervising and teaching the student.
- Assisting the student to achieve their placement learning outcomes.
- Facilitate the student’s development of knowledge and understanding of nursing practice skills.
- Provide the student with formative feedback on their progress.
- Assessing the student’s progress towards competence.
- Designate time to discuss the student’s progress.
- Role & responsibilities of Student:
It is the responsibility of the student to:
-
- To develop an action plan to provide the starting point for discussion with their supervisor at the beginning of the nursing / OT practice placement.
- To identify personal learning objectives pertinent to the placement and client-group.
- With reference to the students stage of training - to practice within the confines of contemporary School of Nursing / Occupational Therapy guidelines/participation levels.
- To reflect on their progress and provide evidence to support achievement of the outcomes/competencies.
- To identify their needs regarding role and responsibilities in terms of safe practice within the care-environment.
Useful resources
Suggested reading
Medications and dementia: https://
Covert Medication: https://
The Mental Capacity Act: https://
Deprivation of Liberty at a glance: https://
The Mental Health Act: https://
What do laboratory tests mean: https:/
Management of Behavioural and Psychological Symptoms (BPSD) in dementia: including Delirium: https://
Information on the various types of Dementia
Please use this link to Alzheimer’s Society website to read about Dementia before starting your placement, You will find it useful and it will help you understand a little and make sense of what you see in that first week of placement:
https://
Read through the sections pertaining to the following:
- Dementia with Lewy Bodies
- Vascular dementia
- Frontotemporal dementia
- Alzheimer’s
- Young onset dementia
- Mixed Dementia
- Alcohol related (Korsakoff) dementia
Video links
Measuring vital signs: https://
Calculating and recording a NEWS score: https://
Suggested template for writing clinical notes
- Observations: are they on general, 15 mins, 1-1 eyesight, 1-1 arms length and has this been reviewed
- Mental Health Act Status: Informal, Section 2, section 3, section 5(2), Section 5(4)
- Mood/ mental state: Predominant emotion over shift e.g. euthymic (normal non-depressed, reasonably positive mood), apathetic, angry, apprehensive, elated, extremely sad & wishing to end life, extremely happy. Current observed emotional state. labile, reactivity (blunted or flat to reactive), & appropriateness
- Diet and Fluids: amount offered and or consumed, the amount of fluids consumed. Whether they needed assistance with feeding and drinking? Any choking concerns / swallowing concerns
- Behaviour and Interactions: how do they present, interact with others, does noise bother them? How are the when others are close? Do they initiate conversation? How is their communication, can they express themselves (expressive dysphasia), do they understand what is said to them (receptive dysphasia). What have they been doing during the day? Wondering / sat for periods. Profile on ward? Have they remained in their bedroom or spent time in the communal areas.
- Engagement in Activities: What activities have they been offered? Did they participate? If so, how long for and what was there engagement like? Activities do not have to be planned activities by the activities coordinator. This could be simple things like 1:1 time / conversations with staff, taking a patient for a therapeutic bath / shower, nail painting, watching their favourite film or listening to their favourite music, engaging with their memory box with the patient etc.
- Physical health: NEWs, BM scores, changes in physical health status, samples taken, tests/scans done (bloods, ECG, external such as x-ray), bowels open?
- Personal care / Activities of Daily Living: what help did they need if any and by how many, what did they do themselves. Bowels open if incontinent?
- Medications: was it accepted, what was refused if any, are they on covert meds and what method worked
Glossary of terms
#NOF – Fractured Neck of Femur.
4AT – A delirium assessment tool. This would be completed in Ward Round.
Abbey Pain Scales – as assessment tool for measuring pain in people with dementia who may not be able to clearly articulate or verbalise their needs.
ABC chart – is an observation tool that helps to understand the causes of behaviour which may present as challenging, by recording what happened before, during and after the behaviour.
ACE 111/ Mini ACE – A diagnostic screening tool for the detection of Dementia or mild cognitive impairment.
ACL’s – Allen Cognitive Level is an assessment that provides a description of the patients’ level of occupational function, their ability to perform familiar activities and learn new ones. This assessment is completed by an Occupational Therapist.
AMHP – Approved Mental Health Practitioner
BM’s – Blood Glucose Monitoring
CD – Controlled drug
CHC – Continuing Healthcare is a package of care for adults aged 18 or over which is funded by the NHS. Sometimes this is sourced by the NHS or Adult Social Care.
CMHT – Community Mental Health Team
CPA – A meeting to assess, plan, review and coordinate the range of treatment, care and support needs for a patient on our ward.
CPN – Community Psychiatric Nurse
CSDD – The Cornell Scale of Depression in Dementia was specifically developed to assess the signs and symptoms of major depression in people living with Dementia.
De- escalation – Using techniques both verbal and non-verbal to reduce agitated and aggressive behaviour.
DHTT – Dementia Home Treatment Team
DNACPR – Do Not Attempt Cardiopulmonary Resuscitation.
DoLs – This a procedure that protects a person receiving care whose liberty has been limited by checking this is appropriate and in their best interest.
ECG – Electrocardiogram (monitors Rhythm and Activity of the heart)
Formulation – Formulation is a process of piecing together information we've gathered through our assessments. A formulation can help us to see how the separate bits of information link together, and help us to see the whole picture, and hopefully understand the patient and their needs in more detail.
HTT – Home Treatment Team
Informal – An informal patient is someone who has capacity and has agreed to an inpatient admission to a Mental Health Hospital.
LCH – Lincoln County Hospital
LPOA - A power of attorney is a way of giving someone you trust the legal authority to make decisions on your behalf if you're no longer able to make them yourself. There are 2 types of LPOA, one for making financial decisions and one for making health and care decisions.
MCA – Mental Capacity Act
MDT – Multi-disciplinary Team
MHA – Mental Health Act
MSU – Midstream Specimen of Urine (Urine Sample)
NIC – Nurse in charge
NICE – The National Institute for Health and Care Excellence. NICE guidelines are evidence-based recommendations for health and social care sector, developed by independent committees, including professionals and lay members.
NOK – Next of Kin
NPI – The Neuropsychiatric Inventory is a tool for capturing behavioural changes in Dementia. The score is reviewed weekly in Ward Round and helps provide an evidence base for prescribing of anti-psychotic medication.
NR – Nearest Relative
OOH – Out of Hours.
PMVA/RRP – Prevention and Management of Violence and Aggression / Reduction of Restrictive Practices
PRN – Pro Re Nata (as and when needed)
RC – Responsible Clinician
ReSPECT – Personalised recommendations for a person’s clinical care and treatment in a future emergency in which they are unable to make or express choice.
Section 17 Leave – This allows patients detained under the Mental Health Act a leave of absence from hospital, this is subject to specific leave conditions in their leave care plan.
SPA – Single Point of Access
Sskins – is an assessment tool to aim in preventing pressure damage. It focuses on 5 keys areas, these are S- Skin integrity, S – Surface, K- Keep moving, I-Incontinence and N – Nutrition.
TTO- To take out medication (for home leave or discharge)
Site maps
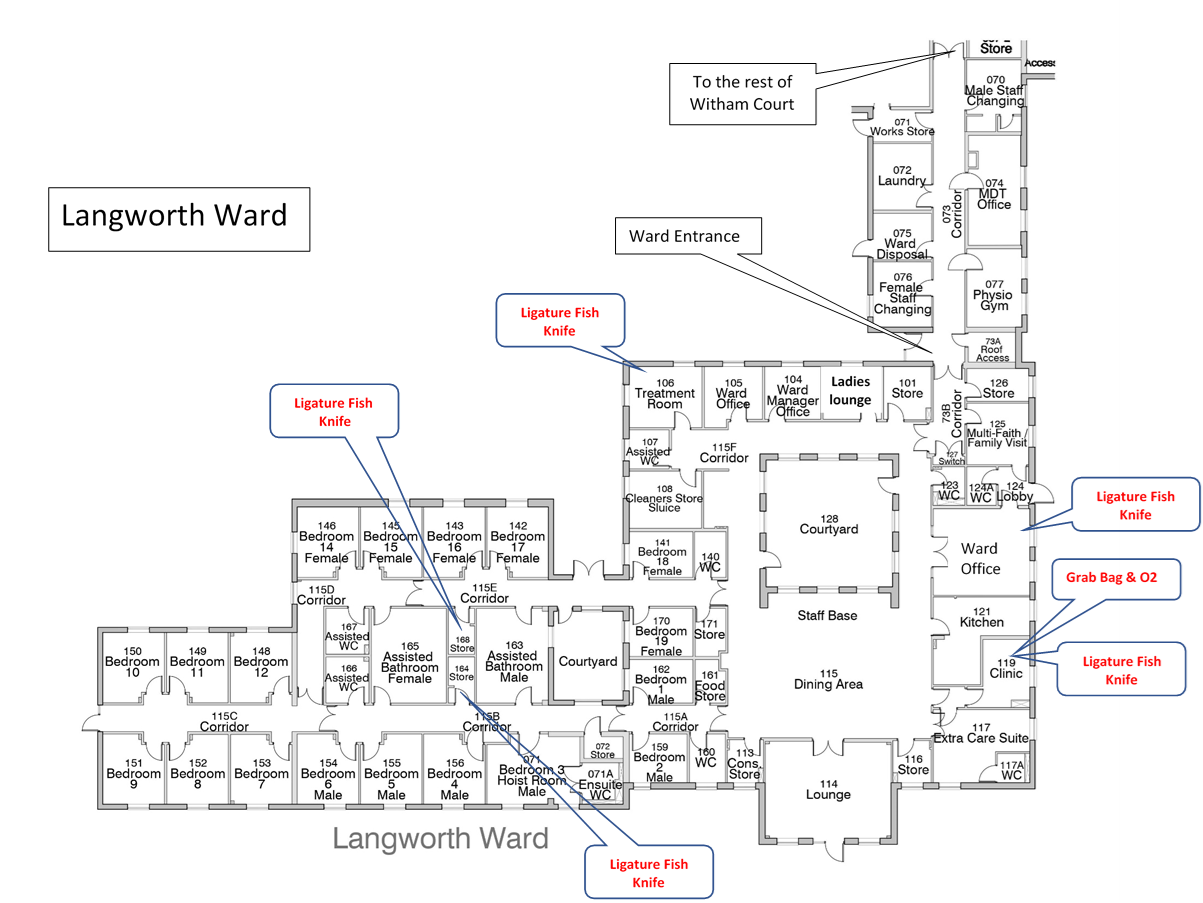
How to find us
Langworth Court & Witham Court
Fen Lane
North Hykeham
Lincoln
LN6 8UZ
Telephone: 01522 508318