Self-help information for patients
Introduction
Being diagnosed with ME / Chronic Fatigue Syndrome (CFS) can feel confusing as there continues to be much debate around what causes it and what maintains it. This information has been put together by the Lincolnshire Specialist ME / CFS Team and is based on many years of both practice based and evidence based experience treating and enabling many young people and adults to improve their health and levels of functioning.
Our hope is that this booklet will give you some basic information around the current understanding we have about the condition prior to starting a treatment programme. If you can stabilise your symptoms by implementing the ideas in this booklet it will enable you to get the most benefit from the full treatment programme when you start this with a therapist. The treatment programme goes in to more depth, so this booklet is only aimed at giving you some positive initial information and strategies to help you manage your health more effectively.
A condition with many names
Myalgic Encephalomyelopathy (ME), Post Viral Fatigue Syndrome (PVFS), Chronic Fatigue Syndrome (CFS) and more recently the American term SEID (Systemic Exertion Intolerance Disease) are some of the names used to describe a syndrome (i.e. where you experience a number of symptoms). A primary feature of all of these names is excessive fatigue. ME / Chronic Fatigue Syndrome is the generally preferred term. It is officially recognised both by the World Health Organisation, NICE and the Equality Act (DoH 2007).
ME / CFS affects people in different ways and no two people experience the illness in the same way. The main common feature is persistent physical and/or mental fatigue, which differs from normal tiredness. It is not adequately relieved by rest or sleep and is usually out of proportion to the activity undertaken.
A range of other symptoms often accompany the fatigue. These include muscle and/or joint pain, headaches, swollen glands and recurring infections such as sore throats. Some people have feelings of dizziness and temperature fluctuations.
There is frequently difficulty with concentration and short term working memory and many people experience problems with their sleep, either struggling to stay awake or feeling” tired but wired” and unable to switch off.
People often report vivid dreams and generally wake feeling un-refreshed. Many people also describe gut problems such as Irritable Bowel Syndrome (IBS) and can develop sensitivities to some foods and medicines.
Currently there is no specific diagnostic blood test for ME / CFS, however there is a clear protocol that is used to confirm the diagnosis. A diagnosis is made by excluding around 40 other conditions that cause fatigue. Your GP will have arranged a variety of blood tests, including liver function tests and routine biochemistry tests, prior to attendance at our specialist clinic, in order to rule out other likely causes of fatigue.
How did I get ME / CFS?
There are some essential and connected structures in the body which together are called the Hypothalamic Pituitary Adrenal (HPA) axis. These are vital in managing and maintaining the body’s homeostasis(3) (the body’s ability to keep itself in balance with hormonal regulation and central and autonomic nervous system regulation). Fatigue and pain in ME / CFS is probably driven by a central sensitisation of the central nervous system (CNS).
Below is a working model of ME / CFS that can be used to explain some reasons why CFS/ME may develop and how the condition is maintained:
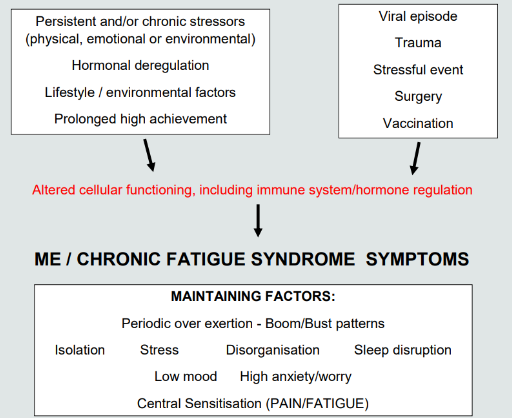
Quite often people report an illness (such as flu or glandular fever) or surgery or a major life stress as triggering ME / CFS. This is understandable as these things can cause a change in the body’s systems which, especially if severe or if there are other pressures, makes it difficult for the body to re-regulate itself again. Continuing to feel unwell or fatigued causes ongoing stress and worry, and further contributes to a vicious cycle that can be difficult to escape from alone.
Knowledge is power! Your understanding of the possible factors influencing and maintaining ME / CFS is vital. The following are some initial strategies we know to be helpful in getting you back in control of your health and wellbeing.
Strategy No.1: Stabilising daily
What is energy?
“Energy is everything.” - Albert Einstein
This is an interesting question and continues to be hotly debated, but new science is looking at ways to further understand our energy system(s). But for the purpose of this booklet we shall focus on the chemical energy known as ATP (adenosine triphosphate). This is what fuels the batteries in our cells known as mitochondria that give us a steady source of energy. The food we eat plus the air we breathe creates the fuel or energy our body needs to keep functioning. So good nutrition, good breathing and posture are really important… more about this later!
Energy is used by the body in many ways so we encourage people to think of everything they do as using their body’s energy. Physical, Mental, Social and Emotional activity all require a use of energy. Even our environments have an effect on our energy. If you are sat down but also chatting or watching TV or just thinking, you are still using energy. So the first thing to start considering is how you use your daily energy in all of these areas. Energy is not just used on the physical tasks we do each day.

Stabilising your daily energy is essential. This means attempting to find a workable balance between the demands of the day (i.e. what you physically have to do and also how you are feeling mentally and emotionally) and the supply of energy available to meets those demands.
A key rule of thumb is to ask yourself each day “Can I do what I am asking myself to do today on most days?”… If your immediate answer is No!... then it is helpful to consider how you can balance what you have to do, what you need to do and what you want to do.
With a condition like ME / CFS there is a tendency to get in to what is described as a “Boom/Bust” pattern of activity. Many people experience the “Bust” days and so start to make the most of the “Boom” days to cram everything in. This cycle is unhelpful as it perpetuates the dysregulation of energy (ATP) and adds to feelings of sickness. Over time this Boom/Bust becomes increasingly exaggerated so even small amounts of “Boom” activity can cause a “Bust”. So moderating this pattern both physically, mentally, emotionally and socially helps in regulating energy cycling and is critical for improving daily energy and stabilising symptoms.
Emotion and Energy
Many people describe living very busy and active lives before becoming unwell with ME / CFS. As a result of symptoms, activity levels significantly reduce or change and this can be a huge challenge emotionally. Most people still have to handle both the expectations they have of themselves and the expectations of others. Commonly people report feelings of frustration, guilt and anxiety as a natural response to not being able to perform or meet their needs and the needs of others at the pace they are used to.
Worry can increase for many reasons but this is also hugely energy draining. Short-term worry can be useful in that it helps us resolve a problem. However, it can also be useless when a situation ‘is what it is’ and there is nothing you can do at this moment to change it. It has been said that one day of worrying about useless worries can use the equivalent energy of a whole week at work!
It is important to be kind to yourself and offer yourself the same level of understanding and good advice that you would offer a best friend going through a similar experience.
Emotions are part of being human but they are primarily driven by our thoughts, which use energy too and can be contributing factors in your day to day energy levels. This would be the same for anyone experiencing a period of ill health no matter what the condition. So we very much encourage you to try and prioritise some pleasure in your days, no matter how small, to counterbalance the stress you are currently experiencing. Pleasure creates positive energy.
What a lot of people fail to recognise is the powerful link between the way you feel emotionally and the effect that this can have on your body and how you feel physically. Recognising this is helpful not because ME / CFS is a psychological problem, but it is a “whole system” problem and being emotionally strong helps heal and rebalance the body.
Thoughts underpin all of our emotions. A positive thought will result in neurochemical signals that boost the body, plus make us feel better emotionally. Conversely, negative thoughts produce altered bodily signals that can be draining. It is easy to get stuck in a negative vicious circle, but spirals can go in 2 directions!
Thinking can either help us to be and feel more resourceful and proactive about managing our health and life commitments or frustrated, angry or guilty which is less helpful and creates more fear, worry and stress.
All emotions are normal expressions (or signals) of how we are feeling inside. So because experiencing ME / CFS can be challenging on all levels we thoroughly encourage people to try and prioritise fun and pleasure. People tend to prioritise their available energy to do what they feel they have to do and neglect time for themselves or a pleasurable activity no matter how small. This can lead to feeling like you are just “existing” in your life rather than “living” your life and contribute to a vicious cycle of fear, resentment and ill health.
Constantly pushing yourself will only add to symptoms, lower your mood and make you feel worse physically, mentally and emotionally.
We use the term being healthily selfish. You need to prioritise your needs as best you can to help your body start to heal and regain its natural balance and functioning.
New agendas
It may help you to consider that in many ways your body is not trying to harm you by creating the unpleasant symptoms of CFS/ME, it is a self-healing organism and may well be trying to get you to change the way you have previously been leading your life to help regain its natural rhythms.
It may be helpful to look at the way you were living your life before becoming unwell as this might have had some contribution to getting ME / CFS, in much the same way as being overly stressed can contribute to many illnesses. Nowadays many people recover from many of these conditions over time by following some key guidelines for health and wellbeing and this can also be good news for recovery from ME / CFS, however we encourage ways of speeding this up.
Imagine if you bought a new plant from the garden centre and it said it needed a sunny position, lots of water and a specific alkaline soil. If you only had space in a dark dry acidic part of the garden it wouldn’t be long before that plant became diseased and failed to thrive. We are organisms much the same as plants and need healthy environments that suit us to thrive.

A significant number of people report that starting to improve and regain healthy functioning happens in small steps. Changing the habits and patterns we have learned for living our lives can be challenging. But consider this… If you keep doing what you have been doing and you are no better then you need to try a new plan. The important thing is to be kind to yourself and give yourself time to figure out what small changes you can start to make to help you manage your energy better and get back in to the control seat of your life. Small changes done every day can equal big changes long term.
Taking to bed and over resting
When we initially become poorly we may have no option but to rest to allow the body some healing time. However beyond 6 weeks too much rest can start to contribute to worsening of symptoms. When the body over-rests, particularly when lying down, muscles can start to become weak and they go through a process of de-conditioning. This process is similar to someone who has been going to the gym and then suddenly gets flu and is laid up in bed for a few weeks. Not surprisingly, when they return to the gym, they cannot manage the level of exercise that they did prior to being unwell. If the person eases themselves back into their routine they should be able to return to their previous level of fitness over time. Unfortunately the demands of life often do not allow us the necessary time to recover before we are pushing ourselves back in to our daily activities.
When you are experiencing ME / CFS your body may have been resting for a considerably long time and therefore experienced some significant de-conditioning and become weaker; muscles start to lose their bulk and stamina significantly reduces. Minimal exertion can lead to breathlessness and achy muscles that feel very weak. Experiencing this can be anxiety provoking and dispiriting. Thus returning to your previous activity levels can feel very difficult.
How to start making progress
As part of the ME / CFS rehabilitation programme you will learn how to build your activity tolerance at safe and manageable levels. To start with, everyday activities (e.g. moving around your home) are the best initial forms of exercise, especially when spaced with times of sitting and relaxation. Following this we use a restorative exercise model which is a gentler form of exercise and includes improving posture, core strength and gentle movement through stretching, Qigong(7), Tai chi(7), Yoga(8) and Pilates(9) exercise
principles. This then allows the body to start rebuilding from a stronger baseline.
We are not suggesting that you do not rest at all, but do consider the adverse effects of taking yourself to bed for long periods of time. We would very much encourage periods of restorative rest within the day, using a wide range of relaxation techniques and/or mindfulness(6) which can be very healing for the body and mind. Sitting down but watching TV or reading might be resting your body but it is not resting your mind.
The most important thing is to establish a consistent and sustainable routine that will allow for a balance between activity and rest. Aim for a slow increase in your activity levels over time, without an increase in fatigue.
Lifestyle/Activity management including Pacing and Grading Activity
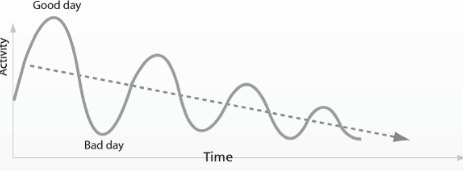
Diagram A
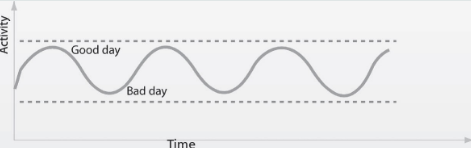
Diagram B
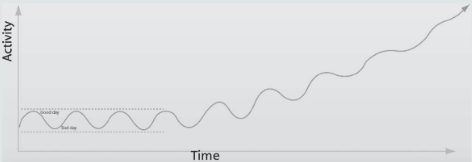
Diagram C
Key points:
- We need a healthy environment to thrive.
- Stabilising and then rebuilding our energy takes time. But developing new habits will boost and maintain health and energy.
- Energy is not all about physical tasks... we use a great deal of energy through our thoughts, emotions and socialising. Try to avoid the boom/bust energy pattern (diagram A) as this can often lead to progressive ill health.
- Focus on getting a consistent and sustainable level of activity (diagram B) with periods of restorative rest within the day. So that might mean reducing activity on a "good day".
- Only gradually increase what you do (diagram C) in small weekly increments. Movement and gentle or restorative exercise (stretching, walking, Yoga, Pilates, Tai chi, Qi Gong) can be helpful.
Strategy No.2: Managing and improving sleep
Are you over-sleeping or struggling to sleep?

Difficulties with sleep, either not being able to stay awake, not being able to fall asleep or early or frequent waking is common for many people at various points in their lives. However when it becomes more persistent it can usually be a result of a multitude of factors that may be either related to lifestyle, a period of illness, pain or high levels of stress and anxiety.
The following tips can be useful tools in calming the mind and this will sooth the stress system aiding natural sleep:
- Go through this checklist below, which is based on the best research evidence to date, to help get you back in to good sleep cycles.
- Reduce electronic stimulation at least an hour before bed. Particularly computers and mobile phones which radiate “blue” light similar to daylight, which acts as a stimulant.
- Dim the lights in the room you are in before bed to help the brain release the “sleepy” hormones (melatonin, serotonin, and tryptophan).
- Reduce caffeine intake after 2pm as caffeine is a stimulant and stays in our system for up to 10 hours, so maybe try decaffeinated or herbal drinks… valerian or chamomile can be helpful relaxants.
- Avoid sleeping in the day beyond a brief catnap, as this will interfere with the body’s natural circadian clock. It’s best to try either a mindfulness breathing technique or some breathing or relaxation exercises if you need a mental rest.
- A worry book can be a useful way of writing down all the “to do’s” or “what ifs” that the mind can throw at us when we get in to bed and it has our full attention. Write your worries down before bed then once in bed say “the day is done, time to sleep, I’ll deal with these tomorrow”. Then try this next technique:
- 10-1 counting. As soon as your head hits the pillow you need to effectively “bore your brain to sleep”. So using a slow in-breath and slow out-breath in your mind say 10…. then repeat with 9….then 8…etc., until you get to 1, then go back to 10 if you are not asleep. If half way through slow breathing and counting your mind becomes distracted with a thought… just notice it… and redirect your attention back to the number 10 and continue… repeat each night until your brain recognizes this as a pattern of initiating sleep. If you wake in the night, just start counting as soon as you wake to tell your brain it just needs to go back to sleep… it’s a very powerful technique if you persist.
- Avoid eating too much before bed, but a light snack can sometimes help. A warm milky drink or a warm bath can help to trigger the sleepy hormones before bed.
- Regular gentle exercise during the day can help aid sleep at night. However vigorous exercise before bed (with the exception of sex) can sometimes affect falling asleep as the brain is over stimulated.
- Try and get into a sleep ritual. Our brain loves routine and regular patterns so it can run this automatically for us.
- Learning to manage and switch off daily stress, worry and anxiety is often key as a brain with too much unresolved “threat” is likely to keep us awake in the early hours.
- Before bed think of 3 positive things that happened in your day, no matter how small, and 3 things you are grateful for…
- Make sure your sleep environment is right, the room temperature is right, mattress comfy, take all digital devices out of the bedroom, use blackout curtains and declutter.
- Turn the clock around… You may need to get up at a certain time but there is no need to look at the clock until the alarm goes off… tempting as this may be, it will likely just wind you up, stopping sleep even more.
- If you don’t fall asleep until the early hours try to still get up at a set time as this helps to keep your circadian clock in a pattern. If you sleep on until mid-morning you will likely disrupt your Circadian rhythm(1) and this will mean you will be unlikely to fall asleep at your desired time at night. Sometimes lying in bed with your eyes open can help and if they want to shut force them to stay open for another few minutes until they are so desperate to shut it allows sleep to follow…
- The 20 minute rule: if you don’t fall asleep straight away get up and find a comfy dimly lit space to sit and read or relax but try not to over stimulate yourself, then when you start yawning or feel tired just try to go to bed again. This way we are helping program the brain to know bed is for sleep, not worrying or tossing and turning.
- If you try all these things and find yourself still awake you could reframe the fact you are still awake as “bonus hours” to practice some relaxation techniques or remember a happy memory. The harder we try to sleep the less it comes…so stop trying and just accept it will come if you “let go of the need for it”… just accepting the fact you are awake but using the time for something else that’s positive can create a win/win and take your mind off feeling frustrated.
- Don’t give up… insomnia or broken sleep is a symptom of an underlying issue, if you can figure out what it is address it, using these techniques you will soon find your way back to good restorative sleep.
- If you are sleeping excessively (i.e. more than 10 hours within a 24hour day) it is important to understand that you are likely misreading fatigue as ‘tiredness’ (there is a difference). You will need to slowly reduce your sleeping by either going to bed a little later or getting up a little earlier. Managing fatigue is not made better by sleeping more and will only add to symptoms. Tiredness can be improved by a normal sleep pattern of no more than 7-9 hours for an adult.
 “Sleep is like a Dove which has
“Sleep is like a Dove which has
landed near one’s hand and stays
there as long as one does not pay
any attention to it; if one attempts
to grab it, it quickly flies away.”
- Victor Frankl
Strategy No.3: Nutrition
“Let food be your medicine and let medicine be your food.” - Socrates

Gut health is a very important factor in your overall health. The Gut is now often referred to as “The second brain” and contains as many neurons as the brain! 90% of our happy chemicals (serotonin) are made in the gut and approximately 60% of the immune system is linked to the gut, hence the term “misery guts”.
If you have heart burn, reflux, bloating, IBS (constipation and/or diarrhoea) it may well be that your gut needs some help to get into better balance. Improving gut health will then improve both your mood and your immune system.
The microbiome(5) of our gut is key to it’s health and is very individual; there is no one size fits all. The following is some general advice that you may find helpful. However, if your gut problems are severe and you are experiencing debilitating IBS or bloating it may be worth asking your GP for a referral to a Dietician, to look at a more specialised diet for you such as the FODMAP(2) Diet.
The importance of hydration

Increasing your fluid intake can make a significant difference to fatigue levels and headaches. Water is best but if you can’t drink water try diluted squash or juices with more water. Adding fresh fruit to water can make a tasty refreshing and healthy addition.
What sort of diet should I be on if I have ME / CFS?
Our guts are very individual, but some general advice we normally suggest is that people with ME / CFS try and make sure they have a healthy balanced diet. This means that you should be eating a variety of carbohydrate (bread, cereals, pasta, rice, potatoes); protein (meat, fish, milk, cheese, eggs, beans); fruit and vegetables. Complex carbohydrates such as brown rice, sweet potatoes, wholegrains and brown pasta are much better for you as they give you a slow release and steady source of energy from the food you eat throughout the day. Eating little and often can be less taxing on the body and reduce after meal slumps.
What about sugary food?
It is helpful to avoid sugary food. This is because sugar contains minimal nutritional value and gives you only a short burst of energy followed by an energy “low” which can make managing your daily energy more difficult.
Are there foods I should eat more of?
There is some evidence that magnesium rich foods such as green leafy vegetables and pulses are helpful. Equally foods high in B vitamins are helpful and for some people low iron stores are associated with fatigue. Iron can be found in: all meats, oily fish, shell fish, egg yolk, dried fruits, and fortified breakfast cereals. Iron absorption is increased by vitamin C. Vitamin C is also important for a healthy immune system and to deal with the stress the body goes through with ME / CFS. Vitamin C can be found in: fruits especially citrus fruits, berries, tomatoes, kiwis, dark green vegetables and potatoes. We would therefore recommend that you try and include these in your diet.
Are there foods that I should exclude from my diet?
There is no conclusive evidence yet that excluding a food will make individuals with ME / CFS better, but some people have found that excluding certain foods has helped. If you want to try and exclude a food we suggest that you do this with guidance from your doctor or a dietician as there are risks of causing more harm than benefit.
What should I do about caffeine, alcohol and energy drinks?
Although many people think these help them cope with the day, they are a very short term solution and actually contribute to the body’s stress system. So the advice is to minimise caffeine and avoid sugary fizzy energy drinks. Many people report that they cannot tolerate alcohol when they become unwell with ME / CFS, so naturally avoid it. However, if you find you are using alcohol as a coping strategy and this is above recommended daily or weekly guidelines, it may be worth discussing this further with your GP or one of our team.
Strategy No.4: Managing Stress

Stress is a part of everyday life and can come in many forms: physical stress (illness, overdoing things), mental stress (having too much to think about or deal with), emotional stress (ruminating and worrying), social stress (dealing with people) or environmental stress (unhealthy living or working conditions).
As human beings we are well designed to deal with stress in short bursts and this is actually good for us and part of keeping our immune system healthy. However when we start to experience more long term stress this can start to negatively affect the body’s systems, particularly the HPA axis(4). The brain is the central organ of stress regulation. When the body/mind is under persistent stress this will take a great deal of the body’s resources and detract from how well the immune system can function, leaving us vulnerable to viruses and illnesses.
The HPA axis is a neuroendocrine system and involves the interaction of the brain structure known as the hypothalamus, the pituitary gland (just below the hypothalamus), and the adrenal glands (at the top of the kidneys). These three pieces of anatomy work in collaboration with our thinking processes to regulate the stress response, which affects our mood, digestion, immune response, libido, and energy usage.
Signs of stress
Not everyone experiences obvious stress symptoms and even within an individual the symptoms might vary in severity and variety, depending on the overall circumstances at the time. It is important to know that stress may not always be easy to recognise - it may be ‘hidden’ and have subtle effects on you. Our body is designed to protect us; therefore anything we interpret as a Threat will activate our stress system. This can be unhelpful thoughts, persistent worries, pushing ourselves too hard, dealing with stressful people and/or situations constantly or just feeling physically unwell day to day.
Below is a list of symptoms which can be part of a stress reaction which are a direct result of the Limbic Centre (our emotional/survival centre) in our brain interpreting a “threat”. Remember this threat may be either real or imagined… if you think a threat thought such as “I can’t cope…” your body reacts in the same way as if you were actually dealing with a threatening situation.
If you are frequently experiencing the symptoms listed below it could indicate that your stress system is heightened and contributing to the symptoms of ME / CFS. Starting to manage stress more effectively can help you to stabilise your symptoms so you can start to get back in control of your health and well-being.
It is also important to recognise that these symptoms can be primarily caused by other things besides stress, but good stress management will help the body stabilise and cope better.
| Physical symptoms | Cognitive symptoms |
|---|---|
|
Tense achy muscles, particularly shoulders and neck Frequent headaches Nausea Diarrhoea or constipation Heart palpitations Shallow breathing Frequent illnesses Dizziness Menstrual irregularities Increased tiredness Unrefreshing sleep |
Racing mind Struggling to switch off Forgetfulness Poor short term or working memory Struggling to concentrate Word finding difficulties |
| Emotional symptoms | Behavioural symptoms |
|---|---|
|
Anxious Moody Feeling overwhelmed Unhappy Irritable Worrying a lot |
Sleep problems (over sleeping or insomnia) Isolating yourself Procrastinating Nervous habits (nail biting, jiggling legs, unable to sit still) Over eating or not eating |
Some good stress management techniques to consider trying are:
- Learning to meditate or do some restorative relaxation
Research has shown the powerful effect restorative relaxation can have on our health and wellbeing. Calming the mind and body can help increase resilience and strengthen the immune system. A few minutes of practice per day can help ease symptoms. There are now many free APPs available or alternatively relaxation CDs are relatively inexpensive; the key is finding one you like and will commit to listening to as much as possible
- Breathing deeply
When stressed there is a tendency to breathe more shallowly and from the upper chest which can add to symptoms of dizziness and fogginess. Good diaphragmatic breathing is very under-rated and can significantly help ease fatigue and pain. Taking a 5-minute breathing focused break can help. Sit up straight, eyes closed, with a hand on your belly. Slowly inhale through your nose for a count of 5 and exhale for a count of 5. Repeat this slowly and rhythmically for 5 minutes and then see how you feel. You may like to repeat a soothing word in your mind such as “relax” or “calm”.
- Be present and focus on the things you can control
When life gets overwhelming it is helpful to focus our daily attention on the things we can control and influence and try to minimize the impact of the things we can’t control.
For 5 minute periods in the day try to slow down both your thoughts and physical movements and practice trying to be present in the moment. It is so easy in our busy lives to be always focused ahead of ourselves or looking backwards at the past and forgetting to live in the moment of now.
Take 5 minutes to really focus on an activity… perhaps notice how the air feels on your face when you’re walking and how your feet feel as they walk on the ground, or enjoy the texture and taste of each bite of food, or observe something in your garden. Notice the vivid colours, shapes or movement. When you really spend time in the moment and focus on your senses you should start to feel less tense.
- Reach out
Your social network may be one of your best tools for handling stress. Talk to others, preferably those who you feel really supported by, face to face or at least on the phone.
- Tune into your body
Mentally scan your body to get a sense of how stress affects you each day. Lie on your back, or sit with your feet on the floor. Start at your toes and work your way up to your scalp, noticing how your body feels and try to identify areas of tension. The neck and shoulders are particular areas where we can hold tension.
Simply be aware of those areas where you feel tight or loose without fear or trying to change anything, and for 1 to 2 minutes, imagine each deep breath flowing to that body part and softening it. Repeat this process as you move your focus around your body, paying close attention to sensations you feel in each body part.
- Self soothe
If circumstances or illness is making you suffer, try not to add to this by being too hard on yourself, show yourself some kindness!
Make time for you… even if it’s just 15 minutes to either have a warm bath or try a warm wheat pillow or hot water bottle around your neck and shoulders for 10 minutes. Close your eyes and relax your face, neck, upper chest, and back muscles.
- Laugh out loud
A good belly laugh doesn’t just lighten the load mentally. It lowers cortisol, your body’s stress hormone, and boosts brain chemicals called endorphins, which help your mood. Put on some relaxed or uplifting music, watching a funny film or chatting with someone who makes you smile can help too.
- Get into nature
Research is showing more and more the therapeutic benefits of the natural world. Finding a quiet spot in your garden or park, or even watching a nature programme on TV, can automatically trigger a release of beneficial chemicals into your blood stream, that help calm and soothe and also can help strengthen our immune response.
- Get moving
Restorative exercise, including gentle stretching, Yoga, Qi gong, Tai chi, Pilates and walking, can help ease both mental and physical stress as the brain releases feel-good chemicals.
- Be grateful
An attitude of gratitude can help increase happiness and resilience in times of adversity. So you could consider keeping a gratitude journal each day, to help you to focus on some of the (often small but significant) things that are good in life that can often be overlooked.
Strategy No.5: Coping with Brain Fog
People are often most disturbed by the mental symptoms of CFS. Symptoms such as forgetting names or getting words mixed up can lead to fears that you have dementia or that you are less intelligent.
When “the fog” descends it can be a very distressing symptom to experience. However it is commonly experienced by individuals with ME / CFS and it is not linked with brain damage or a dementia.
Factors influencing brain fog:
- Chronic stress: being overwhelmed either physically, mentally emotionally or socially.
- Poor sleep; either over sleeping or insomnia.
- Lack of movement: movement helps feed the brain the oxygen it needs to function.
- A high level of anxiety/worry/stress affects the healthy functioning of the short term or working memory.
- Mentally never “switching off”. Focusing on too many things at once.
- Low mood.
The energy required by the brain is remarkable. Your brain is only 2% of your body weight but consumes 20% of your available energy. The brain has an estimated one hundred billion nerve cells, therefore adequate blood flow and oxygen supply are crucial. Emotional energy used by either consciously churning over emotions without resolution or blocking them from conscious thought can use up considerable energy. Multi-tasking is bad for us…nature did not intend us to work like this… the brain works better focusing on one thing at a time.
Strategies that may help:
- Apply the principles of grading/pacing to concentration and memory.
- Reduce stimulants i.e. caffeine, alcohol.
- Eat a healthy balanced diet with a good amount of essential fats.
- Manage stress, try to resolve worries.
- Get your sleep patterns better regulated.
- Identify the time of day you are at your best and use this for demanding mental tasks.
- Make sure your environment is suitable, not too bright, loud or cold/hot.
- Make sure there are minimal distractions.
- Regular restorative exercise helps supply of oxygen glucose and nutrients to the brain!
- Use a Dictaphone or your mobile phone to record things you need to remember.
- Delegate or share responsibilities with family or friends.
- Change tasks frequently, alternate physical and mental tasks.
- Rehearse/repeat things you want to remember.
- If you start losing concentration, don’t slog on… have a break!
- Meditation, regular relaxation of the mind pays huge dividends!
- Games can improve concentration, such as crosswords, puzzles, Sudoku… but remember to pace these activities!
Coping with setbacks
“If you fall down 9 times but get up 10… you’re doing ok.”
Most people with ME / Chronic Fatigue Syndrome will experience setbacks or flare-ups. There can be times when symptoms worsen for a period of time. During these times it can be difficult to maintain your levels of activity.
Different things will provoke setbacks, and they may last for varying lengths of time. Each person will have different ways of dealing with a setback. We would encourage you to become aware of the things that provoke a setback for you, and to develop a plan for coping with a setback when it happens. Do not blame yourself, be kind to yourself and give yourself time to figure out what might help. Setbacks may happen; think of it as a problem to be solved.
What provokes a setback?
Setbacks don’t always have clear-cut causes, but there are a number of things which can contribute to one:
Overdoing it (physically, mentally, emotionally or socially). This may be the result of taking on too much, or simply as a result of doing one activity for too long. Setbacks can be triggered if you are frequently in a boom/bust pattern.
Stress - A period of physical, mental or emotional stress in your life may provoke a setback. Be aware of those things that upset you and spot the signs that you are becoming unduly stressed. Stress management strategies may be especially helpful at these times.
Periods of illness - Following a bout of illness, you may be more prone to a setback. Remember to give yourself time to recover from the illness and then gradually restart activities and exercise by pacing yourself.
Low mood/seasonal factors - Many people find that there is an interaction between their frame of mind and their energy levels. Remember energy and emotion go hand in hand. The lower light and grey days can impact on our mood and in turn on energy levels. Exposure to natural daylight, even in winter, or via the use of a light lamp can help.
Not all these factors apply to everyone. However, taking time to reflect and become aware of the possible factors that may cause your setbacks can be useful to help you work out how to best avoid or minimize these factors.
Even with the best of planning, it may be impossible at times to avoid a setback. But it can be a valuable opportunity to reflect and learn from what may have triggered it. Remember knowledge is power and our body is always trying to give us signals to get us to help it. Maybe by sitting back and quietly reflecting on what happened you might find another piece of your body’s complex jigsaw puzzle of health and wellbeing.
Boosting energy and wellbeing
The following are some reminders of useful strategies that may help:
Relaxation: Remember the importance of proper, recuperating and restorative relaxation within your daily routine. Try a variety of relaxation techniques to see what you like best.
Activity: It’s tempting to stop completely when you are fatigued - don’t – try to get a balance and keep the body moving. Pace your daily activity (mental, physical and emotional) as best you can. Try to get outside at least once a day.
Prioritise: Put your energy into the most important areas of your life first. Try to keep some energy each day to do activities you enjoy.
Compromise: Are you asking too much of yourself at present? Don’t be afraid to step back and reconsider your expectations during a setback. Remember to recognise what you are achieving!
Socialise: If you’re very tired, it’s easy to feel like isolating yourself. Remember that being in touch with someone can be helpful, so what about giving someone a ring, or inviting a friend round?
Pamper: If the going is tough, pace yourself and give yourself a break. If a massage or relaxing shower or bath helps, why not?
Thinking: Remember the way we think influences how we feel. In the midst of a setback it is easy to dwell on what’s not ok. Try to be aware of this, and try out different ways of thinking that are kinder to you and encourage you to know this will pass.
Not all these strategies will apply to you, and you may have developed some additional ideas for successfully managing or reducing the length of a setback. We hope that the information in this booklet enables you to start thinking of how you can start to stabilize your health and well-being. The subsequent treatment programme we offer can help you to then learn how to safely increase your levels of functioning.
Definition of terms
(1) Circadian rhythm
Your circadian rhythm is basically a 24-hour internal clock that is running in the background of your brain and cycles between sleepiness and alertness at regular intervals. It's also known as your sleep/wake cycle. A part of your hypothalamus (a portion of your brain) controls your circadian rhythm.
(2) FODMAP diet
Evidence base has shown a FODMAP diet can be helpful for some patients with conditions such as Irritable Bowel Syndrome (referral to a qualified dietician advised).
(3) Homeostasis
Homeostasis refers to the ability of the body or a cell to seek and maintain a condition of balance or stability within its internal environment when dealing with external changes. It is involved in the maintenance of the constant internal environment which includes the function of kidney, liver, skin, etc.
(4) HPA axis
HPA axis is an abbreviation for a subsystem in your body called the hypothalamic-pituitary-adrenal axis. It describes a complex set of interactions between two parts of the brain—the hypothalamus and the pituitary glands—and the adrenal (or suprarenal) glands that are located at the top of each kidney.
(5) Microbiome
A community of microorganisms (such as bacteria, fungi, and viruses) that inhabit a particular environment and especially the collection of microorganisms living in or on the human body Your body is home to about 100 trillion bacteria and other microbes, collectively known as your microbiome.
(6) Mindfulness
Mindfulness is a very simple form of meditation that was little known in the West until recently. A typical meditation consists of focusing your full attention on your breath as it flows in and out of your body. Mindfulness is about observation without judgement; being compassionate with yourself and focusing on the present moment.
(7) Qigong & Tai chi
Qigong & Tai chi are mind-body-spirit practices that improve mental and physical health by integrating posture, movement and breathing technique.
(8) Yoga
Yoga is an ancient form of exercise that focuses on strength, flexibility and breathing to boost physical and mental wellbeing. The main components of yoga are postures (a series of movements designed to increase strength and flexibility) and breathing.
(9) Pilates
Pilates is a system of exercises using special apparatus, designed to improve physical strength, flexibility, and posture, and enhance mental awareness.
Contact us
To get in touch with the Lincolnshire ME/CFS Service, please email lpft.lincscfs-meservice@nhs.net or call 01476 464046.
Useful websites
Action for ME
Charity run for people with ME/CFS. Information and benefits advice.
www.actionforme.org.uk
The British Association for ME/CFS
www.bacme.info
Moodzone
Practical information, interactive tools and videos from the NHS to help you look after your mental health and avoid common problems like depression and anxiety.
www.nhs.uk/conditions/stress-anxiety-depression
Get self help
Practical self-help for managing stress, worry and low mood.
www.getselfhelp.co.uk
National Institute for Health and Care Excellence (NICE) guidelines for ME/CFS
www.nice.org.uk
If you would like this leaflet in another format, such as Braille, large print or audio, please contact the Communications team at lpft.communications@nhs.net.
Every effort has ben made to ensure that the information in this leaflet was correct at the time of print. However, changes in law may mean that in time some details in this leaflet may be out of date.
Anyone using our services will be treated with dignity at all times and their faith and cultural needs will be accommodated where practically possible.
The Trust is fully compliant with the Data Protection and Confidentiality: NHS Code of Practice requirements.
Published May 2022

